Healthcare Privacy Beyond HIPAA 2
Healthcare privacy bigger than just HIPAA 2. This exploration delves into the multifaceted world of patient data protection, revealing the critical areas extending beyond the familiar confines of HIPAA regulations. We’ll uncover emerging concerns, evolving technologies, and international perspectives, offering a comprehensive understanding of the expanding landscape of healthcare privacy.
The current healthcare system, while reliant on HIPAA, faces significant challenges in a rapidly changing technological environment. This comprehensive overview investigates the evolving nature of data breaches, patient rights, and interoperability, highlighting the limitations of current regulations and the necessity for a more holistic approach to healthcare privacy.
Scope of Healthcare Privacy Beyond HIPAA 2
HIPAA 2, while a significant advancement, doesn’t encompass all facets of healthcare privacy in today’s interconnected world. The rapid evolution of technology, global interconnectedness, and emerging concerns demand a broader perspective on protecting sensitive patient information. This exploration delves into the parameters of healthcare privacy beyond the HIPAA 2 framework, highlighting emerging concerns, technological influences, and international implications.The expanding digital landscape of healthcare necessitates a more comprehensive approach to privacy.
Simply adhering to HIPAA 2 is no longer sufficient. Patient data is increasingly vulnerable to breaches and misuse in various contexts beyond the traditional doctor-patient relationship, necessitating a multifaceted approach to safeguard sensitive information.
Parameters of Healthcare Privacy Beyond HIPAA 2
Beyond the core provisions of HIPAA 2, healthcare privacy encompasses a wider array of considerations. This includes, but isn’t limited to, the use of patient data in research, the sharing of information with third-party payers and administrators, and the security of data stored in cloud-based systems. It also includes the growing concerns around the use of artificial intelligence (AI) in healthcare and the potential for bias in algorithms.
Emerging Privacy Concerns in Healthcare Not Addressed by HIPAA 2
Several emerging privacy concerns in healthcare aren’t adequately addressed by HIPAA
2. These include
- Data breaches in connected medical devices: The increasing use of wearables and other connected medical devices creates new avenues for data breaches. These devices often lack robust security protocols, leaving patient information vulnerable.
- Data sharing with third-party research entities: The use of patient data for research purposes often necessitates sharing information with external entities. These collaborations need robust privacy safeguards to ensure data security and patient consent.
- AI bias in diagnosis and treatment recommendations: AI algorithms used in healthcare may reflect biases present in the data they are trained on, potentially leading to inaccurate or discriminatory outcomes. This raises serious ethical concerns about fairness and equitable access to healthcare.
- Data security in cloud-based storage: Healthcare providers increasingly store patient data in cloud-based systems. However, the security and privacy of data in these systems are frequently subject to scrutiny. Potential vulnerabilities related to data breaches and unauthorized access are significant concerns.
- Patient access and control over their data: Patients need greater control over their data, including the ability to access, correct, and delete their information. HIPAA 2 needs to be enhanced to address these requirements, especially as the digital age advances.
Evolving Technological Advancements Influencing Healthcare Privacy
Technological advancements have a profound impact on healthcare privacy beyond HIPAA 2’s scope. Examples include:
- Rise of telemedicine: Telemedicine facilitates remote consultations and monitoring, increasing the need for secure communication channels and data protection measures.
- Use of wearables and connected devices: The proliferation of wearables and connected devices generates massive amounts of data, requiring new approaches to data management and privacy.
- Artificial intelligence (AI) in healthcare: AI’s role in diagnosis, treatment planning, and drug discovery raises concerns about data security and algorithmic bias.
- Blockchain technology: Blockchain offers potential solutions for secure data sharing and interoperability, but its adoption requires careful consideration of privacy implications.
International Regulations and Standards Impacting Healthcare Privacy Beyond HIPAA 2
International regulations and standards play a crucial role in shaping healthcare privacy beyond HIPAA 2. For instance, the EU’s General Data Protection Regulation (GDPR) sets high standards for data protection and patient rights. This necessitates a global perspective on data privacy and compliance. Countries and regions with stricter data privacy laws will influence the standard of practice worldwide.
Key Differences Between HIPAA 2 and Broader Healthcare Privacy Concepts
| HIPAA 2 Aspect | Beyond HIPAA 2 Aspect | Elaboration | Example |
|---|---|---|---|
| Focus on covered entities | Focus on all healthcare data holders | HIPAA 2 primarily targets entities directly involved in patient care. Beyond HIPAA 2, the scope expands to encompass data collected, processed, or stored by research institutions, technology companies, and third-party payers. | A research lab using patient data without HIPAA compliance. |
| Emphasis on electronic protected health information (ePHI) | Inclusion of all types of patient data | HIPAA 2 primarily addresses electronic health records. Beyond HIPAA 2, considerations extend to data stored in physical records, wearable devices, and other sources. | Protecting data from a patient’s wearable device. |
| US-centric approach | Global and international standards | HIPAA 2 is primarily focused on the US legal framework. Beyond HIPAA 2, consideration must be given to international regulations and standards like GDPR. | A US hospital sharing patient data with an EU-based research institution. |
Data Security and Breach Prevention
Beyond HIPAA’s core principles, robust data security in healthcare demands a proactive approach to threats evolving far beyond simple breaches. The increasing reliance on electronic health records (EHRs) and the growing volume of sensitive patient data make healthcare organizations prime targets for cyberattacks. This requires a comprehensive strategy that transcends HIPAA compliance, addressing emerging vulnerabilities and anticipating future risks.Protecting patient data extends beyond simply adhering to HIPAA regulations.
A holistic approach involves recognizing the multifaceted nature of cyber threats and implementing preventive measures to anticipate and mitigate these dangers. This includes not only technical safeguards but also crucial elements of security awareness training and incident response planning.
Potential Data Breaches Beyond HIPAA’s Scope
Healthcare data breaches can originate from various sources, including malicious actors, insider threats, and even system vulnerabilities. Beyond the traditional phishing scams and malware attacks, modern threats exploit vulnerabilities in software updates, third-party vendors, and poorly secured remote access points. These vulnerabilities are often not addressed by HIPAA alone. For instance, a breach could stem from a compromised third-party vendor managing the EHR system, exposing vast amounts of patient data.
Similarly, sophisticated ransomware attacks, aiming to encrypt and hold data hostage, can significantly disrupt healthcare operations.
Evolving Cyber Threats Impacting Healthcare Data Security
Cyber threats are constantly evolving. The sophistication of malware, the frequency of ransomware attacks, and the increased reliance on remote work environments create new avenues for unauthorized access to patient data. Sophisticated social engineering tactics, like impersonating hospital staff to gain access to networks, are on the rise. Moreover, the use of artificial intelligence (AI) in cyberattacks is becoming more prevalent, allowing attackers to automate and personalize their attacks more effectively.
These threats require organizations to adapt their security strategies continuously.
Best Practices for Enhancing Data Security Measures Beyond HIPAA 2 Compliance
Beyond HIPAA’s requirements, robust data security strategies must incorporate multi-layered defenses. Regular security assessments, penetration testing, and vulnerability scanning are crucial to identify and patch weaknesses in systems. Furthermore, strong access controls, including multi-factor authentication (MFA), and robust data encryption are essential for protecting sensitive information at rest and in transit.
- Regular Security Audits: Conducting regular security audits and penetration testing allows healthcare organizations to identify potential vulnerabilities in their systems and networks, enabling them to proactively address weaknesses before they are exploited. These audits should encompass both internal systems and external access points.
- Employee Training and Awareness: Comprehensive training programs for all employees, including administrative and clinical staff, on security best practices and recognizing phishing attempts are crucial. This includes educating employees on the risks of social engineering tactics.
- Incident Response Planning: Developing and regularly testing a robust incident response plan, including clear procedures for detecting, containing, and recovering from data breaches, is vital. This plan should incorporate communication protocols and escalation procedures for different breach scenarios.
Comparison of Security Protocols for Protecting Sensitive Patient Information Beyond HIPAA 2
Different security protocols offer varying levels of protection against potential threats. For instance, encryption protocols, such as Advanced Encryption Standard (AES), are essential for securing data both at rest and in transit. Network segmentation and firewalls provide further protection by isolating sensitive systems and limiting unauthorized access. Robust access control mechanisms, including MFA, help mitigate the risk of unauthorized access, regardless of whether the attack targets a user or the system itself.
| Security Protocol | Description | Strengths | Weaknesses |
|---|---|---|---|
| AES Encryption | A symmetric encryption algorithm | High security, widely used | Requires secure key management |
| Multi-Factor Authentication (MFA) | Requires multiple forms of authentication | Enhanced security | Can be inconvenient for users |
| Network Segmentation | Dividing a network into smaller, isolated segments | Limits impact of breaches | Requires careful planning and configuration |
Resources for Enhancing Data Security in Healthcare Settings Exceeding HIPAA 2 Requirements
Numerous resources can help healthcare organizations enhance their data security posture beyond HIPAA 2 compliance. These include industry best practices, government guidelines, and security certifications.
- National Institute of Standards and Technology (NIST) Cybersecurity Framework: This framework provides a comprehensive approach to managing cybersecurity risks across various sectors, including healthcare.
- Healthcare Information and Management Systems Society (HIMSS) Security Standards: HIMSS offers resources and best practices tailored to the unique security challenges faced by healthcare organizations.
- International Organization for Standardization (ISO) Standards: ISO standards, such as ISO 27001, provide internationally recognized best practices for information security management.
Patient Rights and Access
Beyond HIPAA’s core principles, patient rights regarding their health information are evolving rapidly. The rise of digital health records and sophisticated data analytics necessitates a broader understanding of patient control over their personal medical data. This evolution demands a proactive approach to patient access, empowering individuals to understand, manage, and utilize their health information in ways that were previously unimaginable.Patient access rights are not static; they adapt to technological advancements and societal expectations.
As healthcare moves increasingly online and into the realm of personalized medicine, patients need more control over their data and the way it is used. This control extends beyond simple access to records and encompasses the ability to correct inaccuracies, understand how their data is used, and even influence the direction of their own health data management.
Evolution of Patient Access Rights
The scope of patient access rights has broadened considerably, spurred by advancements in healthcare technology. Early models focused primarily on access to paper records. Now, patients expect seamless access to electronic health records (EHRs), secure online portals, and the ability to download and share their data in various formats. This shift is not just about convenience; it’s about empowering patients to be active participants in their healthcare journey.
Patient Control Beyond HIPAA 2
Patients’ control over their health information extends beyond the limitations of HIPAA
2. This expanded control includes the ability to
- Request data in different formats, such as mobile-friendly applications or secure cloud storage, facilitating easier access and sharing with other healthcare providers.
- Authorize specific uses of their data, like research projects or data analysis, with clear consent and oversight mechanisms to protect patient privacy.
- Reconsider or amend their health information if they find inaccuracies or outdated details. This right is crucial for maintaining the accuracy and reliability of patient records.
These rights are not just theoretical; they’re becoming increasingly practical as healthcare organizations embrace digital tools and integrate with other systems.
Examples of Expanding Patient Access Rights
Many organizations are implementing innovative approaches to enhance patient access. For instance, some hospitals are offering patient portals that allow patients to access their records, schedule appointments, and communicate with their care team through secure messaging. Additionally, patients are now more empowered to download and share their data with other providers, facilitating continuity of care and streamlining treatment plans.
The adoption of these practices exemplifies a shift toward a more patient-centric approach to healthcare.
Patient Rights Beyond HIPAA 2: A Practical Outlook
| Right | Description | HIPAA 2 Relation | Example |
|---|---|---|---|
| Data Portability | The ability to receive and transmit health information in a usable format. | HIPAA 2 covers some aspects, but the scope is expanding. | Downloading medical records in a PDF or CSV format. |
| Data Control | Ability to control how their health data is used. | HIPAA 2 has limitations on this aspect. | Authorizing specific uses of data for research or analysis. |
| Data Correction | The right to request corrections of inaccurate or incomplete data. | HIPAA 2 allows for corrections but not all cases. | Requesting correction of a wrong diagnosis in the patient record. |
| Data Deletion | Requesting deletion of data under specific circumstances. | HIPAA 2 has stipulations about data deletion. | Requesting deletion of data no longer needed for active care. |
Interoperability and Data Sharing
Healthcare data sharing is crucial for coordinated patient care, but achieving seamless interoperability across different systems presents significant privacy challenges. Beyond the HIPAA framework, ensuring the security and ethical use of patient information shared between providers requires a robust and adaptable approach. This necessitates careful consideration of both the technical and ethical dimensions of data exchange.
Implications of Interoperability on Healthcare Privacy Beyond HIPAA 2
The increasing interconnectedness of healthcare systems necessitates a more nuanced understanding of privacy. Interoperability, while essential for improved care coordination, can inadvertently expose patient data to broader risks if not meticulously managed. This includes the potential for data breaches, unauthorized access, and misuse of sensitive information. The expansion of data sharing beyond a single organization raises concerns about data aggregation and the potential for identifying individuals based on combined information sets.
Healthcare privacy is a complex issue, way beyond just HIPAA 2. Modern data handling, especially when AI is involved, demands more stringent safeguards. For instance, deploying AI code safety measures, like those discussed in Deploying AI Code Safety Goggles Needed , is crucial. Ultimately, ensuring patient data is protected requires a holistic approach, extending beyond current regulations.
Ethical Considerations of Sharing Patient Data Across Different Healthcare Systems Beyond HIPAA 2
Sharing patient data across healthcare systems necessitates a strong ethical framework. Respecting patient autonomy and informed consent becomes paramount. Transparency regarding how data is used and shared must be clearly communicated to patients. Ensuring patient control over their information, including the right to access, correct, and delete data, is critical. Data minimization principles, focusing on collecting only the necessary information, must be rigorously applied.
This approach protects patient privacy while enabling effective data sharing.
Challenges in Ensuring Privacy During Data Sharing Beyond HIPAA 2
Several challenges impede seamless and secure data sharing. Legacy systems with varying data formats and security protocols create obstacles. Ensuring data integrity and confidentiality during transmission is essential. Addressing the complexities of data governance across diverse healthcare organizations presents significant challenges. Compliance with evolving regulations and standards, as well as the need for robust audit trails, are also key challenges.
The complexity of patient data also presents challenges to security, and the risk of errors in transmission or processing must be mitigated.
Detailed Procedure for Securing Data Exchange Between Different Healthcare Providers Beyond HIPAA 2 Guidelines
A secure data exchange protocol should incorporate multiple layers of protection. Firstly, encryption of data both in transit and at rest is essential. Access controls, employing multi-factor authentication and role-based permissions, should be implemented to limit access to authorized personnel only. Regular security audits and penetration testing are crucial for identifying vulnerabilities and enhancing the overall security posture.
Data anonymization and de-identification techniques should be applied where possible to minimize the risk of re-identification. A dedicated team responsible for data security should be established, with clear roles and responsibilities. This ensures a structured and consistent approach to data management.
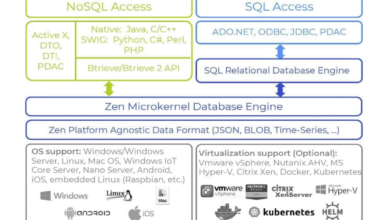
Role of Technology in Enabling Secure Data Sharing Beyond HIPAA 2 Limitations
Modern technologies like blockchain and federated learning offer innovative solutions to enhance data sharing security. Blockchain can create immutable records of data transactions, enhancing transparency and accountability. Federated learning allows for data analysis without sharing raw data, preserving patient privacy. Secure messaging platforms and dedicated data exchange hubs can facilitate secure communication and streamline data flow. The development and implementation of robust encryption protocols and digital signatures can help to protect data integrity and confidentiality.
These technologies can help to ensure the safety and privacy of patient data while promoting efficient and coordinated care.
Privacy in Emerging Technologies: Healthcare Privacy Bigger Than Just Hipaa 2
The landscape of healthcare privacy is rapidly evolving, spurred by the integration of innovative technologies. Beyond the established frameworks like HIPAA, new considerations arise concerning data security, patient control, and ethical implications in emerging technologies. These technologies, while offering potential benefits, introduce unique challenges to maintaining patient confidentiality and autonomy. Addressing these challenges requires a comprehensive understanding of the specific privacy concerns associated with each technology and the development of appropriate regulations and standards.The use of artificial intelligence (AI) and machine learning (ML) in healthcare is transforming diagnosis, treatment, and patient care.
However, these powerful tools raise significant privacy concerns. AI systems often rely on vast datasets of patient information, potentially compromising individual privacy if not carefully managed. Data breaches, biased algorithms, and lack of transparency in decision-making processes are potential risks. Protecting patient data in the context of AI applications requires robust security measures, ethical guidelines, and clear data governance frameworks.
AI and Machine Learning in Healthcare
AI and machine learning algorithms are increasingly used in healthcare for tasks such as diagnosis assistance, personalized treatment plans, and drug discovery. However, these powerful tools rely on vast quantities of patient data, which necessitates robust security measures and clear protocols for data handling. Data anonymization, encryption, and access controls are crucial for protecting patient privacy. Furthermore, the development of AI systems must adhere to ethical guidelines, ensuring fairness, transparency, and accountability in decision-making processes.
Telehealth and Remote Patient Monitoring
Telehealth and remote patient monitoring (RPM) are expanding access to care and enabling continuous health tracking. However, the shift to remote platforms introduces new challenges to maintaining patient privacy. Secure communication channels, robust encryption protocols, and clear guidelines for data storage and access are essential for safeguarding patient information during remote interactions. The use of telehealth platforms should comply with HIPAA regulations and relevant privacy standards.
Furthermore, patients need to be fully informed about how their data is being collected, used, and protected.
Wearable Devices and IoT, Healthcare privacy bigger than just hipaa 2
Wearable devices and the Internet of Things (IoT) are increasingly used for collecting and transmitting patient health data. These devices often collect sensitive information about patients’ daily activities, vital signs, and health conditions. Data security and privacy are paramount, requiring strong encryption, secure data transmission protocols, and clear policies for data storage and access. Patients need to understand the implications of using these devices and be able to control their data.
Genomics and Genetic Data
Genomics and genetic testing are rapidly advancing, providing insights into individual predispositions to diseases. However, genetic data is highly sensitive and raises significant privacy concerns. Robust security measures, strict data access controls, and clear consent mechanisms are essential for protecting this sensitive information. Regulations and standards need to address issues such as data sharing, research use, and potential discrimination based on genetic information.
Stricter ethical guidelines and informed consent procedures are needed.
Privacy Regulations and Standards for Emerging Technologies
Several regulations and standards are emerging to address the unique privacy challenges posed by these technologies. These regulations are aimed at ensuring patient data protection and maintaining trust in healthcare systems. Examples include HIPAA, GDPR, and California Consumer Privacy Act (CCPA). However, these existing frameworks may not adequately address the specific concerns raised by AI, telehealth, wearable devices, and genomics.
A more comprehensive approach is needed that considers the unique characteristics of each emerging technology and develops specific regulations and standards. The development of guidelines specific to AI and machine learning in healthcare is a growing need. Specific guidelines and regulations are necessary to address the unique challenges of data handling, algorithmic bias, and transparency in decision-making.
International and Global Perspectives
Healthcare privacy isn’t confined by national borders. International data flows, the rise of global telehealth, and the increasing interconnectedness of healthcare systems demand a global perspective on privacy regulations. This necessitates understanding how different countries approach patient data protection, the challenges of cross-border data transfer, and the potential for collaborative solutions.The current patchwork of regulations creates complex situations for patients and healthcare providers.
A standardized approach to healthcare privacy is crucial for fostering trust, facilitating collaboration, and ensuring equitable access to care on a global scale. This global approach is critical to the smooth functioning of the international healthcare landscape.
Comparison of Healthcare Privacy Regulations Across Major Regions
Different regions have established unique frameworks for protecting patient data. Understanding these differences is essential for navigating international collaborations and ensuring patient privacy in a globalized healthcare environment.
| Region | Key Privacy Law | Key Differences from HIPAA 2 | Enforcement Mechanisms |
|---|---|---|---|
| European Union (EU) | General Data Protection Regulation (GDPR) | Focuses on data subject rights (e.g., right to access, rectification, erasure) and emphasizes accountability of data controllers. Broader scope than HIPAA, covering various sectors including healthcare. | Independent data protection authorities in each member state, with enforcement powers. Significant fines for non-compliance. |
| United States | Health Insurance Portability and Accountability Act (HIPAA) | Primarily focuses on the protection of health information held by covered entities (e.g., hospitals, clinics). Its scope is primarily domestic. | Office for Civil Rights (OCR) within the Department of Health and Human Services, responsible for investigating and enforcing compliance. |
| Asia-Pacific | Varying regulations (e.g., Personal Information Protection Act of Singapore, Personal Information Protection Law of South Korea). | Different emphasis on specific aspects of data protection. Some focus on consent, others on data minimization. | Varying enforcement mechanisms across different countries, often including data protection authorities. |
| Latin America | Different laws depending on the country (e.g., Brazil’s General Data Protection Law). | Similar to the EU, a growing trend toward comprehensive data protection. Focus on individual rights and data security. | National data protection agencies or similar bodies responsible for enforcement. |
Implications of International Data Flows on Healthcare Privacy
The global exchange of healthcare data presents both opportunities and challenges. Facilitating cross-border collaborations and research can improve patient outcomes. However, different regulations and enforcement mechanisms can complicate data transfers. International data flows in healthcare need to be carefully managed to protect patient privacy.
Healthcare privacy is a complex issue, way beyond just HIPAA 2. Recent developments, like the Department of Justice’s new Safe Harbor policy for Massachusetts transactions, Department of Justice Offers Safe Harbor for MA Transactions , highlight the intricate web of regulations affecting data security. This emphasizes that maintaining patient confidentiality requires a multifaceted approach, encompassing a wider range of legal and technological considerations.
Challenges in Maintaining Consistent Privacy Standards Across Borders
Discrepancies in legal frameworks, varying levels of technical capabilities, and different cultural approaches to privacy make consistent standards challenging to achieve. Cultural norms regarding data sharing can also influence the implementation and enforcement of privacy regulations.
Healthcare privacy concerns extend far beyond HIPAA 2. Recent vulnerabilities in cloud storage, like those highlighted in the Azure Cosmos DB Vulnerability Details , underscore the need for robust security measures beyond just compliance. We need to constantly assess and adapt our strategies to keep patient data safe, even in the face of evolving threats.
Examples of International Collaborations in Healthcare Privacy Beyond HIPAA 2
International collaborations are emerging to address global healthcare challenges. These collaborations are working towards harmonizing privacy standards and facilitating secure data sharing across borders. Examples include initiatives focused on research, pandemic response, and global health security. Many countries have been working together on cross-border data sharing initiatives in specific areas, like pandemics or research.
Public Awareness and Education

Healthcare privacy extends far beyond the familiar confines of HIPAA. As the digital landscape evolves and new technologies emerge, understanding and safeguarding our sensitive health information requires a proactive approach. This necessitates a robust public awareness campaign, ensuring individuals are empowered to protect their privacy rights and understand the implications of evolving privacy concerns.Educating the public about healthcare privacy beyond HIPAA is crucial for fostering responsible data handling and encouraging informed decision-making.
It’s not just about knowing the rules; it’s about understandingwhy* these rules are essential. This proactive approach empowers patients to make informed choices about their data and promotes a culture of respect for healthcare privacy.
Strategies for Educating the Public
Effective public awareness campaigns require multifaceted strategies. These initiatives should target diverse audiences with tailored messages, leveraging various communication channels. Clear, concise language is paramount to ensure comprehension across different demographics. Emphasis on the practical implications of healthcare privacy, such as how it impacts their daily lives, is essential to fostering engagement.
Methods for Increasing Patient Awareness
Patient awareness campaigns should use diverse communication channels. Websites, social media, and community events are effective tools for reaching wider audiences. Interactive tools and materials can help make complex information more accessible and engaging. For instance, easily understandable infographics and short videos can effectively convey intricate privacy concepts. Public service announcements (PSAs) on radio and television can also reach a large segment of the population.
Communicating Privacy Policies
Effective communication of privacy policies is paramount. Policies should be written in plain language, avoiding jargon and technical terms. They should be readily available on websites and in clinics, clearly outlining what data is collected, how it’s used, and who has access. Interactive demonstrations and workshops can be helpful for those who might find it difficult to understand the complexities of privacy policies.
Examples include workshops on how to access and update their health information.
Educational Resources for Patients
Providing accessible and understandable educational resources is vital. These resources should include brochures, pamphlets, and online guides explaining key privacy concepts in simple terms. For instance, a dedicated section on a healthcare provider’s website with FAQs and tutorials on accessing personal health information (PHI) can prove incredibly helpful. Interactive online quizzes and games can reinforce learning and make the subject matter more engaging.
Educational materials should be adaptable to diverse learning styles and preferences.
Ongoing Public Awareness Campaigns
Ongoing public awareness campaigns are essential to address evolving privacy concerns. As technology advances, new threats to healthcare privacy emerge, requiring continuous adaptation of educational materials. Regular updates to existing resources and the development of new ones are crucial. Partnerships with patient advocacy groups and healthcare organizations can enhance outreach and engagement. Examples include collaborations with community centers and schools to disseminate information and address privacy concerns directly.
Last Recap
In conclusion, healthcare privacy extends far beyond HIPAA 2, encompassing a complex web of evolving technologies, international regulations, and patient rights. This discussion underscores the need for a proactive and adaptable approach to safeguarding patient data, ensuring that privacy remains paramount in the ever-changing landscape of healthcare.
FAQ
What are some examples of emerging privacy concerns not covered by HIPAA 2?
Emerging technologies like AI and telehealth introduce new vulnerabilities. Data breaches involving wearable devices and IoT medical equipment are also significant concerns. Additionally, the use of genomic data necessitates specialized privacy protections.
How do international regulations influence healthcare privacy?
Different countries have varying privacy laws, leading to challenges in ensuring consistent standards across borders. International data flows further complicate the issue, demanding international cooperation and harmonization.
What are the key differences between HIPAA 2 and broader healthcare privacy concepts?
A table outlining the key differences will highlight the scope, enforcement mechanisms, and specific areas of concern. This comparative analysis will emphasize the limitations of HIPAA 2 and the broader considerations needed for comprehensive privacy protection.
What are some patient rights beyond HIPAA 2?
Patient rights in the context of emerging technologies need to be addressed. This includes access to, control over, and correction of their health information, considering the increasing use of electronic health records and AI.