Modernizing Endpoint Management Platform Healthcare
Modernizing endpoint management platform healthcare is no longer a luxury, but a necessity. In today’s interconnected world, healthcare organizations face unprecedented challenges in securing and managing their vast network of devices – from laptops and desktops to mobile phones and increasingly complex IoT medical equipment. Outdated systems leave these organizations vulnerable to costly breaches and operational inefficiencies, directly impacting patient care and the bottom line.
This post dives into the crucial need for modernization, exploring the benefits, key features, and strategic implementation of a robust, secure endpoint management platform specifically designed for the unique demands of the healthcare industry.
We’ll examine the stark contrast between legacy systems and their modern counterparts, highlighting how advancements in security, automation, and compliance features offer a significant return on investment. We’ll also discuss the crucial role of remote management, integrated patching, and robust mobile device management (MDM) in a geographically dispersed healthcare environment. Finally, we’ll look ahead to the future, exploring the transformative potential of AI, cloud-based solutions, and other emerging technologies that will redefine endpoint security in healthcare.
The Current State of Endpoint Management in Healthcare
Healthcare organizations are facing a perfect storm of challenges when it comes to managing their endpoints. The increasing reliance on technology, coupled with stringent regulatory requirements and the sensitive nature of patient data, creates a complex and demanding environment. Effectively managing the diverse range of devices – from traditional laptops and desktops to mobile devices, wearables, and a growing number of Internet of Things (IoT) devices – is a significant undertaking, fraught with potential risks.
Challenges in Managing Healthcare Endpoints
Healthcare organizations face a unique set of challenges in endpoint management. The sheer volume and diversity of devices, coupled with the need for robust security and compliance, creates a complex landscape. Legacy systems often struggle to keep pace with the rapid technological advancements, leaving organizations vulnerable to security breaches and operational inefficiencies. Furthermore, the geographically dispersed nature of many healthcare providers adds another layer of complexity to endpoint management.
Maintaining consistent security policies and providing timely support across multiple locations can be a significant challenge. The integration of new technologies, such as telehealth platforms and AI-powered diagnostic tools, further complicates the picture, requiring careful consideration of security and data privacy implications. This necessitates a more proactive and comprehensive approach to endpoint management.
Security Vulnerabilities Associated with Outdated Endpoint Management Systems
Outdated endpoint management systems pose significant security risks to healthcare organizations. These systems often lack the advanced security features necessary to protect against modern cyber threats. For instance, inadequate patch management can leave devices vulnerable to malware and ransomware attacks, potentially leading to data breaches and disruption of critical services. Weak authentication mechanisms can allow unauthorized access to sensitive patient data.
The lack of robust endpoint detection and response (EDR) capabilities can hinder the ability to detect and respond to security incidents effectively. Moreover, the absence of centralized management capabilities makes it difficult to enforce consistent security policies across all devices. These vulnerabilities can have severe consequences, ranging from financial penalties to reputational damage and legal repercussions. A recent example of this is the ransomware attack on a major hospital system, which resulted in the disruption of patient care and a significant financial loss.
Inefficient Processes Caused by Legacy Endpoint Management Solutions
Legacy endpoint management solutions often lead to inefficient processes, hindering productivity and increasing operational costs. Manual processes for software deployment and updates are time-consuming and error-prone. Lack of centralized management capabilities makes it difficult to track and manage devices effectively. Troubleshooting issues can be challenging due to the lack of real-time visibility into device status and performance.
The inability to automate routine tasks, such as software patching and security updates, further contributes to inefficiency. This can lead to increased IT support costs and reduced staff productivity. For example, a hospital might spend countless hours manually updating software on hundreds of computers, time that could be better spent on direct patient care.
Impact of Inefficiencies on Patient Care and Operational Costs
The inefficiencies caused by legacy endpoint management systems have a direct impact on patient care and operational costs. Disruptions to critical systems, such as electronic health records (EHRs) and medical imaging systems, can delay diagnoses and treatments, impacting patient outcomes. Security breaches can lead to the loss of sensitive patient data, resulting in reputational damage and legal liabilities.
Increased IT support costs and reduced staff productivity further strain healthcare budgets. The cumulative effect of these inefficiencies can significantly impact the quality of care and the financial viability of healthcare organizations. The cost of downtime due to system failures or security breaches can be substantial, often running into millions of dollars.
Comparison of Legacy and Modern Endpoint Management Solutions
| Feature | Legacy System | Modern System | Improvement |
|---|---|---|---|
| Software Deployment | Manual, time-consuming | Automated, streamlined | Reduced deployment time, fewer errors |
| Patch Management | Manual, inconsistent | Automated, centralized | Improved security, reduced vulnerability |
| Security Monitoring | Limited visibility | Real-time monitoring, threat detection | Enhanced security posture, faster incident response |
| Device Management | Decentralized, difficult to track | Centralized, comprehensive inventory | Improved efficiency, better control |
| Remote Support | Limited capabilities | Robust remote access and troubleshooting | Faster resolution of issues, reduced downtime |
Benefits of Modernizing Endpoint Management Platforms
Upgrading your healthcare organization’s endpoint management platform isn’t just about keeping up with the times; it’s about significantly improving patient care, bolstering security, and streamlining operations. The advantages extend far beyond simple technological updates, impacting every aspect of your digital infrastructure and ultimately, your bottom line. Let’s explore the key benefits in detail.
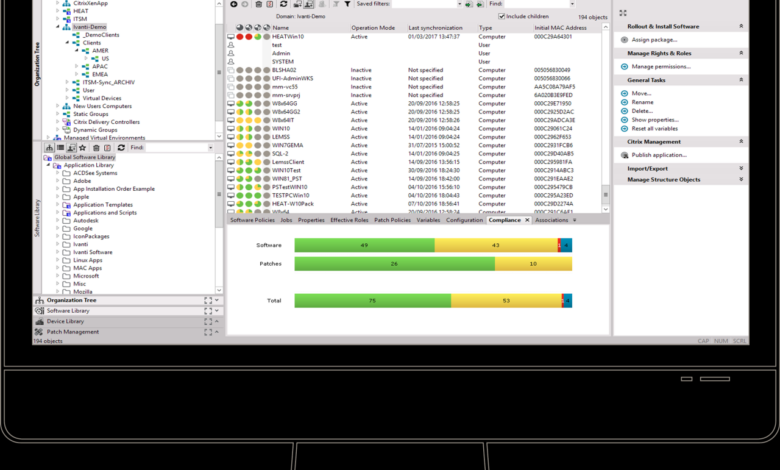
Centralized Endpoint Management in Healthcare
A centralized endpoint management system offers unparalleled control and visibility across all your devices – from desktops and laptops to mobile devices and IoT medical equipment. This unified view allows for streamlined patching, software updates, and configuration management, reducing the complexity of managing a diverse IT landscape common in healthcare settings. Imagine effortlessly deploying security updates across hundreds of devices with a single click, instead of manually updating each one.
This efficiency translates to reduced IT staff workload and improved response times to critical security threats. The ability to remotely monitor device health and performance allows for proactive identification and resolution of issues before they impact patient care or data security.
Improved Security Features
Modern endpoint management platforms incorporate robust security features essential for protecting sensitive patient data. Multi-factor authentication (MFA) adds an extra layer of protection, significantly reducing the risk of unauthorized access. Endpoint Detection and Response (EDR) solutions continuously monitor devices for malicious activity, providing real-time alerts and automated responses to threats. For instance, an EDR system might automatically quarantine a compromised device, preventing the spread of malware across the network.
This proactive approach is crucial in a healthcare environment where data breaches can have severe consequences. These advanced security measures go beyond basic antivirus software, providing a comprehensive defense against increasingly sophisticated cyber threats.
Automation in Streamlining Endpoint Management Tasks
Automation is the cornerstone of efficient endpoint management. Modern platforms automate repetitive tasks such as software deployment, patch management, and user provisioning. This frees up IT staff to focus on more strategic initiatives, such as improving cybersecurity posture or developing innovative solutions to enhance patient care. For example, automating the onboarding process for new employees can reduce the time it takes to get them up and running, minimizing disruptions to workflow.
The automation of routine tasks also reduces human error, leading to fewer incidents and improved overall system stability.
Enhanced HIPAA and Regulatory Compliance
Modern endpoint management platforms play a crucial role in ensuring compliance with HIPAA and other healthcare regulations. Features like data loss prevention (DLP) and access control help organizations meet stringent data security requirements. The centralized logging and auditing capabilities provided by these platforms simplify the process of demonstrating compliance to auditors. For example, the ability to track all access attempts to sensitive patient data provides a clear audit trail, facilitating compliance audits and investigations.
This comprehensive approach to security and compliance reduces the risk of penalties and reputational damage.
Return on Investment (ROI) of Modernization
The investment in modernizing your endpoint management platform yields substantial returns across various aspects of your organization.
- Reduced IT operational costs: Automation and streamlined processes reduce the need for extensive manual intervention, lowering labor costs.
- Improved security posture: Reduced risk of data breaches and associated financial and reputational damage.
- Enhanced productivity: Employees experience fewer IT-related disruptions, leading to increased efficiency.
- Better compliance: Reduced risk of non-compliance penalties and legal issues.
- Improved patient care: Reliable and secure systems ensure uninterrupted access to patient information and medical devices.
Consider a hypothetical scenario: a hospital with 500 endpoints spends an average of 10 hours per week on manual patching and troubleshooting. Modernization could reduce this to 2 hours per week, freeing up 40 hours of IT staff time. At an average hourly rate of $50, this translates to a weekly cost saving of $2000, or $104,000 annually.
This doesn’t even account for the potential cost savings from avoided security breaches or improved patient care. The ROI is clear: modernization is an investment that pays for itself many times over.
Key Features of a Modern Healthcare Endpoint Management Platform
Modernizing endpoint management in healthcare isn’t just about upgrading technology; it’s about bolstering security, improving compliance, and enhancing the overall patient experience. A robust platform is crucial for managing the diverse range of devices used within a healthcare organization, from clinical workstations to mobile devices and IoT sensors. The features described below highlight the key elements that contribute to a secure and efficient healthcare IT environment.
Essential Features for a Secure and Compliant Platform
A modern healthcare endpoint management platform must prioritize security and compliance above all else. This necessitates a comprehensive suite of features designed to protect sensitive patient data and ensure adherence to regulations like HIPAA. Failure to do so can lead to significant financial penalties and reputational damage.
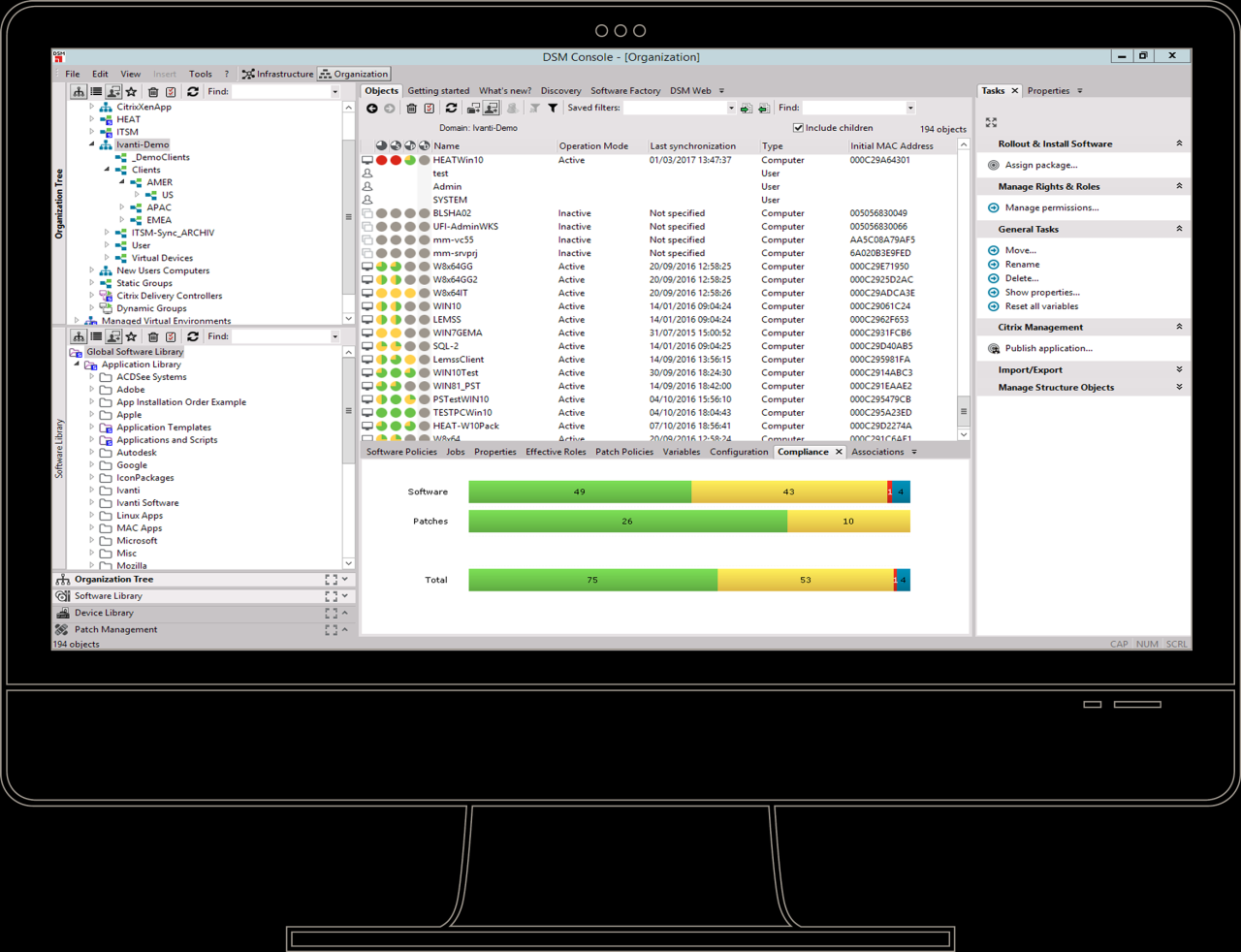
- Centralized Management Console: A single pane of glass offering complete visibility and control over all endpoints, regardless of location or operating system.
- Advanced Security Features: Including multi-factor authentication (MFA), endpoint detection and response (EDR), and data loss prevention (DLP) tools to mitigate cyber threats.
- Automated Patching and Vulnerability Management: Proactive identification and remediation of software vulnerabilities to prevent exploitation.
- Role-Based Access Control (RBAC): Granular control over user permissions, limiting access to sensitive data based on job roles and responsibilities.
- Compliance Reporting and Auditing: Automated generation of reports to demonstrate compliance with relevant regulations and internal policies.
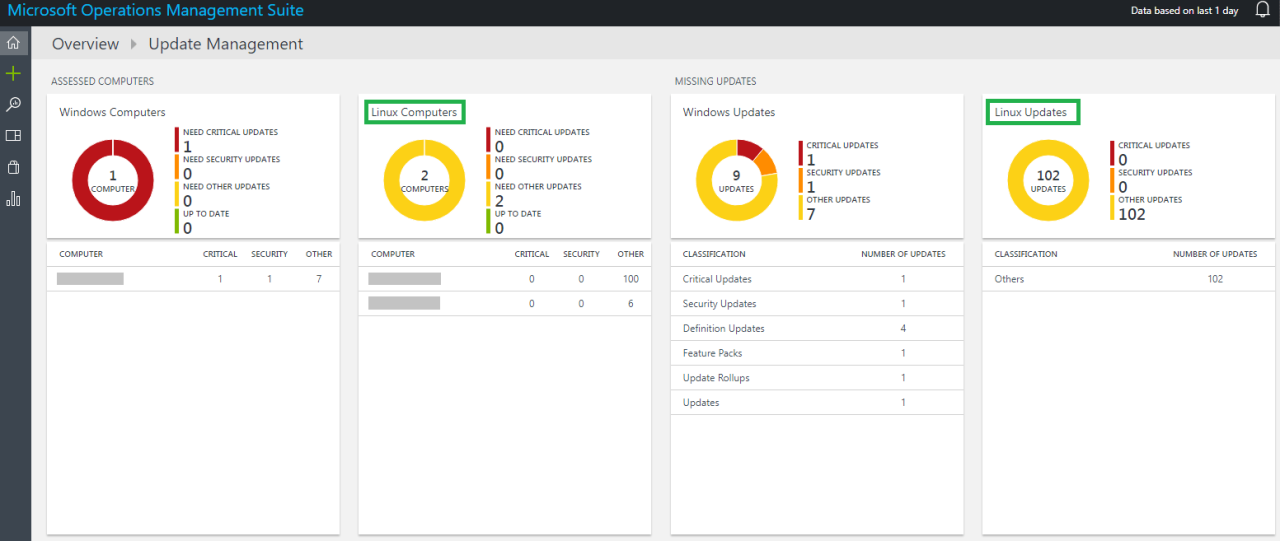
Remote Management Capabilities in a Geographically Dispersed Environment
Healthcare organizations often operate across multiple locations, including hospitals, clinics, and remote offices. Effective remote management is paramount to ensure consistent security and operational efficiency across all these sites.Remote management capabilities allow IT administrators to:
- Deploy software updates and configurations remotely: Reducing downtime and ensuring consistency across all endpoints.
- Monitor endpoint health and performance in real-time: Identifying and resolving issues proactively before they impact patient care.
- Securely access and manage endpoints remotely: Providing support and troubleshooting assistance to users across various locations.
- Enforce security policies consistently across all locations: Maintaining a uniform security posture regardless of geographic dispersion.
For example, a large hospital system with multiple campuses can use remote management to ensure all devices are patched and updated with the latest security protocols simultaneously, minimizing the risk of a widespread cyberattack.
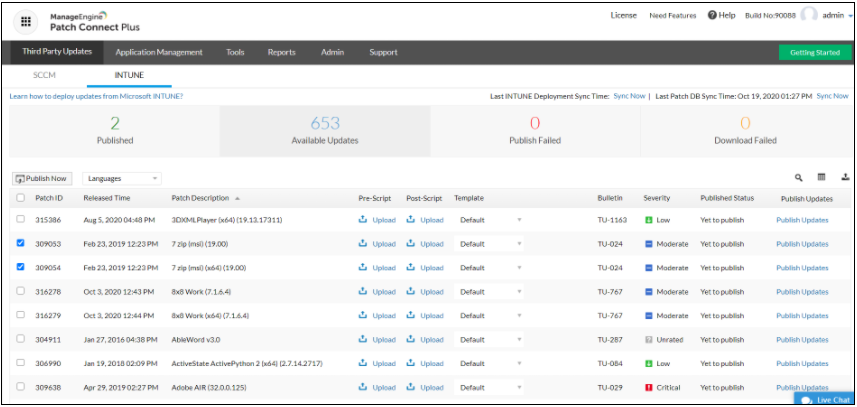
Integrated Patching and Vulnerability Management for Enhanced Security
Automated patching and vulnerability management are critical for maintaining a strong security posture. Manually patching devices is time-consuming, error-prone, and leaves systems vulnerable to exploitation.Integrated patching and vulnerability management tools:
- Automatically identify and prioritize vulnerabilities: Focusing on the most critical issues first.
- Deploy patches automatically to endpoints: Minimizing downtime and ensuring consistent security across all devices.
- Monitor patch deployment status: Ensuring all patches are successfully applied.
- Generate reports on vulnerability remediation: Providing insights into the organization’s security posture.
This proactive approach significantly reduces the risk of successful cyberattacks and ensures compliance with regulatory requirements. For instance, the WannaCry ransomware attack highlighted the devastating consequences of neglecting timely patching.
Robust Mobile Device Management (MDM) Capabilities for Healthcare Workers, Modernizing endpoint management platform healthcare
Healthcare workers increasingly rely on mobile devices for accessing patient data, communicating with colleagues, and managing schedules. Robust MDM capabilities are essential for securing these devices and protecting sensitive information.MDM capabilities should include:
- Device enrollment and management: Securely enrolling and managing mobile devices used by healthcare workers.
- Remote wipe capabilities: Protecting sensitive data in case of device loss or theft.
- Application management: Ensuring only approved applications are installed on devices.
- Data encryption: Protecting sensitive data at rest and in transit.
Effective MDM prevents unauthorized access to patient data and ensures compliance with HIPAA regulations. Consider a scenario where a doctor’s phone is lost; remote wipe capabilities can instantly erase all sensitive patient data on the device.
Secure BYOD (Bring Your Own Device) Policies
BYOD policies can offer cost savings and improve employee satisfaction. However, they also introduce significant security risks if not properly managed. A modern platform must support secure BYOD policies through features such as:
- Conditional Access Policies: Granting access to corporate resources only if the device meets specific security requirements (e.g., device encryption, password complexity).
- Data Segmentation: Separating corporate data from personal data on employee devices to limit the impact of a compromise.
- Mobile Threat Defense (MTD): Detecting and mitigating threats on employee devices.
For example, a hospital might allow nurses to use their personal smartphones for work, but only if they install a specific MDM app and enable device encryption. This balances the convenience of BYOD with the necessity of protecting sensitive patient data.
Implementation and Integration Strategies
Successfully implementing a modern endpoint management platform (EMP) in a healthcare setting requires careful planning and execution. This involves a phased approach that considers the unique complexities of healthcare IT infrastructure, data security regulations (like HIPAA), and the diverse needs of healthcare professionals. A robust strategy ensures minimal disruption to patient care while maximizing the benefits of the new system.
Step-by-Step Implementation Plan
A phased rollout minimizes risk and allows for iterative improvements. The following steps provide a framework:
- Assessment and Planning: Thoroughly assess the current IT infrastructure, identify all endpoints (desktops, laptops, mobile devices, IoT devices), and document existing security protocols. Define project goals, timelines, and resource allocation. This phase includes a risk assessment and the development of a comprehensive communication plan.
- Proof of Concept (POC): Implement the EMP in a small, controlled environment (e.g., a single department) to test functionality, identify potential issues, and refine the implementation strategy before full-scale deployment. This allows for adjustments based on real-world feedback.
- Pilot Deployment: Expand the implementation to a larger group, perhaps a specific hospital wing or clinic, to further validate the solution and identify any scaling challenges. Gather user feedback and address any remaining issues before widespread adoption.
- Full-Scale Deployment: Once the pilot program is successful, roll out the EMP across the entire healthcare organization. This involves installing agents on all endpoints, configuring security policies, and integrating with existing systems. Ongoing monitoring and support are crucial during this phase.
- Post-Implementation Review: Conduct a thorough review of the implementation process to identify areas for improvement and to measure the effectiveness of the new EMP. This data informs future updates and optimizations.
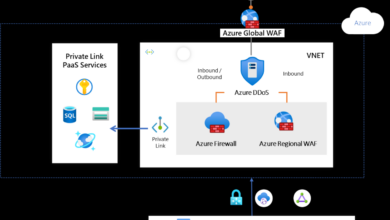
Integration with Existing Healthcare IT Infrastructure
Seamless integration with existing systems is crucial. This involves:
- Directory Services Integration: Integrate the EMP with the organization’s Active Directory or other directory services to automate user provisioning and management.
- Electronic Health Record (EHR) System Integration: Depending on the specific needs, integration with the EHR system might be necessary for certain functionalities, such as access control based on user roles and responsibilities. This integration needs to comply with strict data security and privacy regulations.
- Security Information and Event Management (SIEM) Integration: Integrate the EMP with the SIEM system to centralize security monitoring and incident response. This provides a comprehensive view of security events across the healthcare organization.
- Other System Integrations: Consider integration with other relevant systems, such as help desk ticketing systems, vulnerability management tools, and network monitoring systems. This enhances overall system efficiency and reduces manual intervention.
Healthcare Staff Training
Effective training is vital for successful adoption. This includes:
A multi-faceted approach is necessary, combining different training methods to cater to various learning styles. This could involve instructor-led training sessions, online modules, and hands-on workshops. Regular refresher courses and ongoing support are essential to maintain proficiency and address any evolving needs.
Potential Challenges and Mitigation Strategies
Several challenges can arise during implementation:
| Challenge | Mitigation Strategy |
|---|---|
| Resistance to change from healthcare staff | Effective communication, demonstrating the benefits of the new system, and providing adequate training and support. |
| Integration complexities with legacy systems | Phased integration, thorough planning, and engagement of experienced IT professionals. |
| Data security and privacy concerns | Compliance with HIPAA and other relevant regulations, rigorous security testing, and robust data encryption. |
| Budget constraints | Prioritize functionalities, explore different vendor options, and consider phased implementation to spread costs over time. |
Future Trends in Healthcare Endpoint Management
The healthcare landscape is undergoing a rapid digital transformation, driven by the increasing adoption of connected medical devices, electronic health records (EHRs), and telehealth platforms. This digital expansion necessitates a proactive and sophisticated approach to endpoint management, moving beyond traditional methods to embrace innovative technologies and strategies. The future of healthcare endpoint management will be shaped by several key trends, significantly impacting patient care and operational efficiency.
Artificial Intelligence and Machine Learning in Endpoint Security
AI and ML are poised to revolutionize endpoint security in healthcare. These technologies can analyze vast amounts of data from various endpoints to identify anomalies and potential threats in real-time, far exceeding the capabilities of traditional signature-based security systems. For example, AI algorithms can detect unusual access patterns or data transfers that might indicate a malware infection or insider threat, triggering automated responses like quarantining affected devices or alerting security personnel.
ML models can continuously learn and adapt to evolving threats, enhancing the effectiveness of security measures over time. This proactive approach minimizes the risk of data breaches and ensures the ongoing confidentiality, integrity, and availability of sensitive patient information. Imagine a system that automatically flags suspicious login attempts from a specific IP address based on learned patterns of legitimate user activity, preventing unauthorized access before it can cause damage.
The Impact of Cloud-Based Endpoint Management Solutions
Cloud-based endpoint management solutions offer significant advantages over on-premise systems, particularly in the context of healthcare’s geographically dispersed and often complex IT infrastructure. Cloud solutions provide centralized management and control over all endpoints, regardless of their location, simplifying administration and reducing the need for extensive on-site IT support. Scalability is another key benefit; cloud platforms can easily adapt to changing needs, accommodating growth in the number of endpoints and users without requiring significant upfront investment.
Furthermore, cloud-based solutions often incorporate advanced security features, such as data encryption and access controls, enhancing the protection of sensitive patient data. Consider a large hospital system with multiple clinics across a wide region; a cloud-based solution allows seamless management of all endpoints from a single console, regardless of whether they are located in a hospital, clinic, or even a physician’s office.
Emerging Technologies Shaping the Future of Healthcare Endpoint Management
Several emerging technologies are set to reshape the landscape of healthcare endpoint management. Zero Trust security models, for instance, are gaining traction, focusing on verifying every user and device before granting access to resources, regardless of location. This approach significantly reduces the attack surface and limits the impact of potential breaches. Extended Detection and Response (XDR) solutions integrate security data from multiple sources – endpoints, networks, and cloud – providing a holistic view of the security posture and enabling faster threat detection and response.
Furthermore, blockchain technology holds promise for enhancing data security and integrity by creating an immutable record of endpoint activity and access permissions. For example, a blockchain-based system could track every access to a patient’s electronic health record, providing a verifiable audit trail and enhancing accountability.
Predictions for the Evolution of Endpoint Security in the Next 5-10 Years
Over the next 5-10 years, we can anticipate a significant shift towards AI-driven, proactive security solutions. Traditional signature-based antivirus will become increasingly less effective as cyberattacks become more sophisticated. We expect to see wider adoption of zero trust architectures, XDR solutions, and blockchain technologies, enhancing security posture and resilience. The integration of endpoint management with other IT systems, such as EHRs and telehealth platforms, will become increasingly important, facilitating seamless data exchange and improving operational efficiency.
For example, imagine a scenario where an endpoint management system automatically alerts the EHR system of a potential security breach on a device used to access patient records, enabling immediate action to mitigate the risk.
Anticipated Impact on Patient Care and Operational Efficiency
The modernization of endpoint management platforms will have a profound impact on both patient care and operational efficiency. Improved security will protect sensitive patient data, reducing the risk of breaches and maintaining patient trust. Streamlined administration will free up IT staff to focus on more strategic initiatives, improving overall efficiency. Proactive threat detection and response will minimize downtime and disruptions to services, ensuring the continued delivery of high-quality patient care.
Furthermore, the integration of endpoint management with other healthcare systems will facilitate better data exchange and collaboration, leading to more informed decision-making and improved patient outcomes. For instance, real-time monitoring of medical devices could alert clinicians to potential equipment malfunctions, preventing delays or errors in treatment.
Final Thoughts
Modernizing your healthcare endpoint management platform isn’t just about upgrading technology; it’s about safeguarding patient data, streamlining operations, and ultimately, improving the quality of care. By embracing centralized management, robust security features, and strategic implementation, healthcare organizations can significantly reduce their vulnerability to cyber threats, enhance compliance, and achieve a substantial return on investment. The future of healthcare endpoint management is bright, promising increased efficiency, improved security, and a more resilient healthcare ecosystem.
Let’s embrace the change and build a safer, more secure future for patients and providers alike.
Popular Questions: Modernizing Endpoint Management Platform Healthcare
What are the biggest risks of NOT modernizing my endpoint management system?
Significant risks include data breaches leading to hefty fines, HIPAA violations, operational disruptions, loss of patient trust, and increased vulnerability to ransomware attacks.
How long does it typically take to implement a new endpoint management platform?
Implementation timelines vary depending on the size and complexity of the organization’s IT infrastructure, but generally range from several weeks to several months.
What kind of training is needed for healthcare staff after implementation?
Comprehensive training programs are essential, covering basic usage, security protocols, troubleshooting, and reporting procedures. Hands-on training and ongoing support are crucial for successful adoption.
How can I measure the ROI of a modernized endpoint management platform?
ROI can be measured by tracking reductions in security incidents, IT support costs, compliance penalties, and improved operational efficiency. Quantifiable metrics should be established before implementation to track progress effectively.