Achieving and Maintaining Compliance in Healthcare
Achieving and maintaining compliance in healthcare is a complex but crucial journey for any organization in the medical field. Navigating the intricate web of federal and state regulations, from HIPAA to OSHA and beyond, requires a proactive and comprehensive approach. This isn’t just about avoiding penalties; it’s about building a culture of ethical practice, protecting patient data, and ensuring the highest standards of care.
This blog post will delve into the key aspects of building and maintaining a robust compliance program, from risk assessment to data security and incident response.
We’ll explore practical strategies for implementing effective compliance training, conducting thorough audits, and responding to violations swiftly and decisively. We’ll also examine emerging challenges, such as the impact of telehealth and AI on compliance, and how technology can help us navigate this evolving landscape. Get ready to discover how to build a truly compliant and ethical healthcare organization!
Regulatory Landscape of Healthcare Compliance
Navigating the complex world of healthcare compliance requires a thorough understanding of the numerous federal and state regulations that govern the industry. Failure to comply can result in significant financial penalties, reputational damage, and even criminal charges. This section will explore the key regulations, highlighting their differences and recent changes.
Key Federal and State Regulations Impacting Healthcare Compliance
The healthcare industry is subject to a multifaceted regulatory environment, with federal regulations often setting minimum standards, and state regulations adding further layers of complexity. Key federal regulations include the Health Insurance Portability and Accountability Act (HIPAA), the Occupational Safety and Health Act (OSHA), and the Affordable Care Act (ACA), among others. State regulations vary considerably, often addressing issues such as licensing, certificate of need, and specific patient care standards.
The interplay between these federal and state regulations creates a dynamic and challenging compliance landscape.
Differences Between HIPAA, OSHA, and Other Relevant Regulations
HIPAA, OSHA, and other regulations serve distinct yet interconnected purposes. HIPAA focuses on protecting the privacy and security of protected health information (PHI). OSHA, on the other hand, sets workplace safety standards to protect healthcare workers from hazards. Other relevant regulations might include the Clinical Laboratory Improvement Amendments (CLIA), which regulate laboratory testing, or the Centers for Medicare & Medicaid Services (CMS) regulations, which govern participation in federal healthcare programs.
These regulations, while distinct in their focus, often overlap and require coordinated compliance efforts. For example, a breach of PHI (HIPAA violation) might also expose workers to a safety hazard (OSHA concern).
Examples of Recent Changes in Healthcare Compliance Regulations and Their Impact, Achieving and maintaining compliance in healthcare
The healthcare compliance landscape is constantly evolving. Recent changes, such as updates to HIPAA’s breach notification rules or new regulations related to telehealth security, illustrate this dynamism. For example, the increased use of telehealth during the COVID-19 pandemic led to a surge in cybersecurity concerns and prompted regulatory bodies to update guidelines on securing patient data transmitted electronically. These changes necessitate ongoing vigilance and adaptation from healthcare providers to maintain compliance.
Another example is the increasing focus on data privacy and the implementation of stronger data security measures across all aspects of patient care.
Key Compliance Requirements
Understanding the specific requirements of each regulation is crucial for maintaining compliance. The following table summarizes key aspects of several important regulations:
| Regulation | Key Requirements | Penalties for Non-Compliance | Resources for Compliance |
|---|---|---|---|
| HIPAA | Privacy Rule, Security Rule, Breach Notification Rule; Protecting the privacy and security of Protected Health Information (PHI). | Civil monetary penalties (CMPs), potential criminal charges, reputational damage. | HHS Office for Civil Rights (OCR) website, HIPAA Journal |
| OSHA | Workplace safety standards for healthcare settings, including bloodborne pathogen standards, and hazard communication. | Fines, citations, potential legal action. | OSHA website, professional safety consultants |
| ACA | Requirements for health insurance coverage, provision of certain preventive services. | Financial penalties for non-compliance. | CMS website, legal counsel specializing in healthcare law |
| CLIA | Standards for laboratory testing and personnel qualifications. | Fines, sanctions, suspension or revocation of certificates. | CMS website, CLIA-certified consultants. |
Implementing a Robust Compliance Program
Building a robust healthcare compliance program isn’t a one-time task; it’s an ongoing process requiring consistent effort and adaptation. A strong program minimizes risks, protects patients, and ensures the organization operates ethically and legally. This involves a multi-faceted approach encompassing risk assessment, policy development, staff training, and ongoing monitoring.
Steps in Creating a Comprehensive Healthcare Compliance Program
Developing a comprehensive healthcare compliance program requires a structured approach. First, a thorough assessment of the organization’s specific risks is crucial. This includes identifying potential violations of federal and state regulations, such as HIPAA, Stark Law, and Anti-Kickback Statute. Next, clear and concise policies and procedures must be developed to address these identified risks. These policies should be readily accessible to all staff.
Implementation involves actively integrating these policies into daily operations. Finally, ongoing monitoring and auditing are essential to ensure the program’s effectiveness and identify areas for improvement. Regular reviews and updates are vital to keep pace with evolving regulations and best practices.
Risk Assessment and Mitigation in Healthcare Settings
Effective risk assessment involves a systematic process of identifying potential compliance vulnerabilities. This can be achieved through internal audits, employee surveys, and review of incident reports. Once risks are identified, a mitigation strategy should be developed. This strategy may involve implementing new policies, providing additional training, or enhancing technological safeguards. For example, a hospital might assess the risk of data breaches by analyzing past incidents, employee access controls, and the security of its electronic health record (EHR) system.
Mitigation strategies could include implementing multi-factor authentication, employee security awareness training, and regular penetration testing.
Sample Compliance Policy: Patient Privacy and Data Security
This policy Artikels the organization’s commitment to protecting patient privacy and data security in accordance with HIPAA regulations. All employees are responsible for adhering to this policy. Access to patient information is limited to authorized personnel on a need-to-know basis. Unauthorized disclosure of patient information is strictly prohibited and will result in disciplinary action, up to and including termination.
The organization will implement appropriate safeguards, including physical, technical, and administrative measures, to protect electronic protected health information (ePHI). Regular security audits and employee training will be conducted to ensure compliance. Any suspected breaches must be reported immediately to the designated compliance officer.
Importance of Staff Training and Education in Maintaining Compliance
Staff training is not merely a box to tick; it’s a cornerstone of a successful compliance program. Educated employees are more likely to understand and adhere to policies and procedures, reducing the risk of non-compliance. Comprehensive training programs should cover all relevant regulations, policies, and procedures. Regular refresher courses ensure employees stay updated on best practices and emerging threats.
Interactive training methods, such as case studies and simulations, can enhance learning and retention. Moreover, creating a culture of compliance through ongoing communication and feedback is crucial for long-term success.
Essential Elements of a Successful Compliance Training Program
A successful compliance training program should incorporate several key elements:
- Needs assessment to identify training gaps.
- Development of engaging and relevant training materials.
- Use of multiple training methods (e.g., online modules, in-person sessions, interactive workshops).
- Regular assessments to measure employee understanding and retention.
- Documentation of all training activities.
- Ongoing feedback mechanisms to improve the program.
- Integration of compliance training into new employee onboarding.
- Regular refresher training to address changes in regulations and best practices.
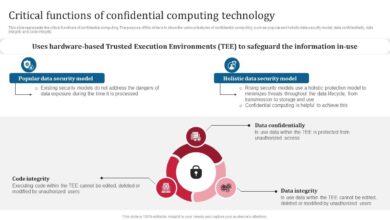
Data Security and Privacy in Healthcare: Achieving And Maintaining Compliance In Healthcare

Protecting patient data is paramount in healthcare. The sheer volume of sensitive information handled, coupled with increasingly sophisticated cyber threats, necessitates a robust and multi-layered approach to data security and privacy. Failure to do so can result in devastating financial penalties, reputational damage, and, most importantly, harm to patients.
Technical and Administrative Safeguards for Patient Data Protection
Effective data security requires a blend of technical and administrative controls. Technical safeguards encompass the technological measures used to protect data, while administrative safeguards focus on policies, procedures, and workforce training. For example, technical safeguards might include strong encryption, firewalls, and intrusion detection systems. Administrative safeguards involve developing and enforcing comprehensive data security policies, conducting regular risk assessments, and providing thorough employee training on data privacy and security best practices.
A well-designed program integrates both, creating a layered defense against data breaches.
Implications of Data Breaches and Response Steps
Data breaches can have severe consequences. Financially, they can lead to significant fines from regulatory bodies like HIPAA in the US and GDPR in Europe, as well as legal costs associated with lawsuits from affected patients. Reputational damage can be equally devastating, eroding public trust and impacting patient acquisition. Operationally, a breach can disrupt services and require significant resources for remediation and recovery.
A swift and effective response is critical. This includes immediate containment of the breach, notification of affected individuals and regulatory authorities, a thorough investigation to determine the root cause, and implementation of corrective actions to prevent future incidents.
Examples of Effective Data Encryption and Access Control Methods
Data encryption is a cornerstone of data security. Methods like Advanced Encryption Standard (AES) with 256-bit keys provide robust protection for data at rest and in transit. Access control, implemented through role-based access control (RBAC) systems, ensures that only authorized personnel have access to specific data based on their job responsibilities. For example, a nurse might only have access to patient records relevant to their assigned patients, while a physician might have broader access.
Multi-factor authentication (MFA), requiring multiple forms of verification (e.g., password and a one-time code), adds an extra layer of security to prevent unauthorized access.
Data Security in the Cloud versus On-Premises Systems
Cloud-based and on-premises systems each offer different security considerations. Cloud providers typically offer robust security infrastructure, including data centers with physical security measures and advanced security technologies. However, responsibility for data security is shared between the provider and the healthcare organization. On-premises systems offer greater control over security but require significant investment in infrastructure and expertise to maintain.
The choice depends on factors such as budget, technical expertise, and the organization’s risk tolerance. A hybrid approach, combining both cloud and on-premises solutions, can offer a balanced solution.
Data Breach Incident Handling Process
The following flowchart illustrates a typical process for handling a data breach incident:[Imagine a flowchart here. The flowchart would begin with “Incident Detection,” leading to “Initial Response (Containment),” followed by “Investigation (Root Cause Analysis),” then “Notification (Affected Individuals & Authorities),” next “Remediation (Corrective Actions),” and finally “Post-Incident Review (Lessons Learned).” Each stage would have brief descriptions, visually represented by boxes connected by arrows showing the flow of the process.
The flowchart visually represents a structured, sequential approach to managing a data breach.]
Auditing and Monitoring for Compliance
Maintaining a strong healthcare compliance program isn’t a one-time event; it’s an ongoing process requiring consistent vigilance. Regular auditing and monitoring are crucial for identifying weaknesses, ensuring effectiveness, and demonstrating a commitment to regulatory adherence. This involves a multifaceted approach encompassing various methods and key performance indicators.
Different Auditing Methods
Effective compliance auditing leverages a variety of methods to provide a comprehensive assessment. These methods offer different perspectives and levels of detail, allowing for a thorough understanding of compliance posture. For example, internal audits provide a first-hand look at internal processes, while external audits offer an independent perspective. Additionally, desk audits examine documentation, while operational audits involve direct observation of processes in action.
A combination of these approaches is often most effective.
Key Performance Indicators (KPIs) for Measuring Compliance Effectiveness
Measuring the effectiveness of a compliance program requires carefully selected KPIs. These metrics provide quantifiable data to track progress and identify areas needing improvement. Examples of relevant KPIs include the number of compliance violations identified, the time taken to resolve identified issues, the percentage of staff completing required compliance training, and the number of successful audits completed without major findings.
Tracking these KPIs over time allows for the identification of trends and the assessment of the overall effectiveness of compliance initiatives. For instance, a consistently high number of violations in a specific area might indicate a need for additional training or process improvements.
Conducting Internal Audits and Addressing Deficiencies
Internal audits are a proactive approach to compliance monitoring. They involve a systematic review of policies, procedures, and practices to identify any areas of non-compliance. The process typically involves planning the audit scope, selecting audit team members, collecting and analyzing data, documenting findings, and developing corrective action plans. Once deficiencies are identified, a prioritized list of corrective actions should be developed, assigned responsibility, and tracked to completion.
Regular follow-up audits are crucial to ensure that corrective actions have been effectively implemented and maintained. For example, if an internal audit reveals inadequate documentation of patient consent, the corrective action might involve providing additional training to staff on proper documentation procedures, implementing a new electronic consent system, and conducting a follow-up audit to verify compliance.
Reporting Mechanisms for Tracking Compliance Issues and Corrective Actions
Effective tracking and reporting are essential for managing compliance issues. A centralized system for documenting compliance issues, corrective actions, and follow-up activities is critical. This system could be a dedicated database, a shared spreadsheet, or a specialized compliance management software. Regular reports summarizing compliance performance should be generated and distributed to relevant stakeholders. These reports should clearly identify trends, highlight areas of concern, and demonstrate progress in addressing identified issues.
For example, a monthly compliance report might summarize the number of incidents, the types of violations, the status of corrective actions, and any recurring issues.
Sample Audit Report Template
A well-structured audit report is crucial for communicating findings and recommendations effectively. The following table provides a sample template:
| Section | Content |
|---|---|
| Audit Objective | Clearly state the purpose of the audit. (e.g., To assess compliance with HIPAA regulations regarding patient data security.) |
| Audit Scope | Define the specific areas and processes covered by the audit. (e.g., Review of electronic health records access logs, employee training records, and security protocols.) |
| Findings | Detail the specific observations and evidence of compliance or non-compliance. (e.g., Insufficient password complexity, lack of regular security awareness training, missing data encryption.) |
| Recommendations | Suggest specific actions to address identified deficiencies. (e.g., Implement multi-factor authentication, provide mandatory security awareness training, encrypt all sensitive data at rest and in transit.) |
| Corrective Actions | Artikel the steps taken to implement the recommendations. (e.g., New password policy implemented, security training scheduled and completed, data encryption implemented and verified.) |
| Conclusion | Summarize the overall compliance status and the effectiveness of corrective actions. |
Responding to Compliance Violations
Responding to a compliance violation in healthcare is critical not only for maintaining patient safety and trust but also for avoiding hefty fines and legal repercussions. A swift, thorough, and documented response demonstrates a commitment to compliance and can mitigate potential damage. This process involves several key steps, from initial identification to long-term preventative measures.
Steps to Take When a Compliance Violation is Identified
Upon discovering a potential compliance violation, immediate action is paramount. First, secure all relevant documentation and evidence related to the incident. This might include patient records, emails, system logs, or witness statements. Next, report the violation through established internal channels, typically to a compliance officer or designated ethics committee. This ensures the issue is handled according to protocol and allows for a coordinated response.
Finally, initiate a thorough investigation to determine the facts and circumstances surrounding the violation. This should be done promptly and impartially to ensure accuracy and fairness.
Importance of a Thorough Investigation Process
A thorough investigation is the cornerstone of effective compliance response. It provides a detailed understanding of the violation’s root cause, extent, and impact. This understanding informs the development of appropriate remediation strategies and helps prevent future occurrences. A comprehensive investigation should include interviews with involved parties, review of relevant documents, and potentially, consultation with external experts. The investigation’s findings should be meticulously documented and preserved as evidence.
Failure to conduct a thorough investigation can lead to inadequate remediation efforts and a higher risk of recurrence.
Remediation Strategies and Prevention of Future Violations
Remediation focuses on correcting the identified violation and its impact. This might involve restoring data integrity, correcting billing errors, or providing additional training to staff. Preventing future violations requires a proactive approach, focusing on addressing the root causes uncovered during the investigation. This could involve implementing new policies and procedures, improving training programs, enhancing technological safeguards, or strengthening internal controls.
Regular audits and monitoring are also essential for ensuring the effectiveness of implemented preventative measures.
Examples of Effective Corrective Action Plans
An effective corrective action plan (CAP) is specific, measurable, achievable, relevant, and time-bound (SMART). For instance, if a violation involves improper disposal of medical waste, a CAP might include: 1) retraining all staff on proper waste disposal procedures; 2) implementing a new waste tracking system; 3) conducting regular audits of waste disposal practices; 4) establishing a clear reporting mechanism for any waste disposal concerns; and 5) setting a deadline for completion of all corrective actions.
Similarly, if a violation involves a data breach, a CAP might include: 1) notifying affected individuals; 2) engaging cybersecurity experts to investigate the breach and implement enhanced security measures; 3) reviewing and updating data security policies; and 4) providing staff with additional cybersecurity training.
Hypothetical Compliance Violation Scenario and Response
Imagine a scenario where a hospital employee accidentally accesses a patient’s medical record without a legitimate reason. Upon discovery, the incident is reported to the compliance officer. An investigation ensues, interviewing the employee, reviewing system logs, and assessing the potential impact on the patient. The investigation reveals the employee lacked awareness of proper access protocols. The corrective action plan includes mandatory retraining on HIPAA regulations, implementing stricter access controls, and conducting regular audits of access logs.
The employee receives counseling, and the hospital reviews its training materials to ensure they are comprehensive and effective. This comprehensive response addresses the immediate violation, educates the employee, and enhances the overall security of patient data.
Emerging Trends and Challenges in Healthcare Compliance

The healthcare landscape is constantly evolving, driven by technological advancements and shifting regulatory priorities. This creates a dynamic environment for compliance, presenting both opportunities and significant challenges. Navigating this complexity requires a proactive and adaptable approach, ensuring organizations remain compliant while leveraging new technologies to improve patient care and operational efficiency. This section will explore some of the key emerging trends and challenges impacting healthcare compliance.
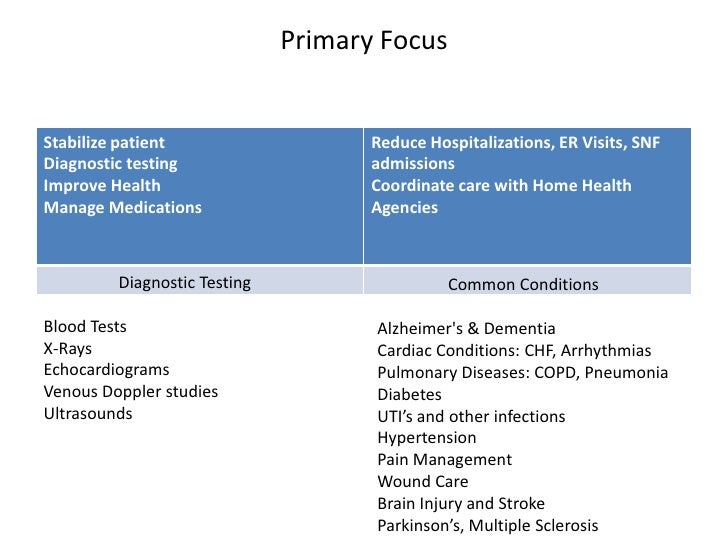
Telehealth’s Impact on Healthcare Compliance
The rapid expansion of telehealth has dramatically altered healthcare delivery, creating new compliance considerations. While offering increased access to care, telehealth introduces challenges related to patient privacy, data security, licensing and credentialing across state lines, and ensuring the appropriate level of care is delivered remotely. For example, a telehealth provider must adhere to HIPAA regulations regarding the secure transmission and storage of patient data, regardless of the location of the patient or provider.
Furthermore, compliance with state-specific licensing requirements for telehealth practitioners needs careful attention to avoid legal issues. Maintaining accurate documentation and ensuring the security of remote patient monitoring devices are also crucial compliance aspects of telehealth.
Challenges Posed by Artificial Intelligence and Machine Learning in Healthcare
Artificial intelligence (AI) and machine learning (ML) are transforming healthcare, offering the potential for improved diagnostics, personalized treatment, and more efficient operations. However, their implementation introduces unique compliance challenges. Bias in algorithms, lack of transparency in decision-making processes, and ensuring the accuracy and reliability of AI-driven diagnostic tools are key concerns. For instance, an AI algorithm trained on biased data may perpetuate existing health disparities, leading to unfair or discriminatory outcomes.
Furthermore, the legal and ethical implications of AI’s role in diagnosis and treatment require careful consideration and robust regulatory frameworks. Establishing clear lines of accountability when AI systems make errors is also a critical challenge.
Emerging Compliance Risks Associated with Big Data Analytics in Healthcare
Big data analytics holds immense promise for improving healthcare outcomes through identifying trends, predicting risks, and personalizing care. However, the use of vast amounts of patient data raises significant compliance concerns. Protecting patient privacy and ensuring data security are paramount, particularly given the increased risk of data breaches and unauthorized access. Compliance with regulations like HIPAA and GDPR requires robust data governance frameworks and security measures.
The potential for data misuse and the ethical implications of using patient data for secondary purposes, such as research or marketing, also require careful consideration. For example, a hospital using patient data for research must obtain appropriate consent and ensure data anonymization to protect patient privacy.
Technology’s Role in Improving Healthcare Compliance
Technology plays a crucial role in both creating and mitigating compliance challenges. While new technologies introduce risks, they also offer powerful tools for enhancing compliance. For instance, electronic health records (EHRs) can improve data accuracy and reduce the risk of human error. Automated compliance monitoring systems can help identify potential violations early on. Blockchain technology can enhance data security and transparency.
However, the implementation of these technologies requires careful planning and integration to ensure they effectively support compliance efforts and do not introduce new vulnerabilities.
Timeline of Key Milestones in the Evolution of Healthcare Compliance Regulations
The evolution of healthcare compliance regulations reflects the ongoing effort to balance innovation with the protection of patient safety and rights. A simplified timeline might include:
- 1996: HIPAA (Health Insurance Portability and Accountability Act) is enacted, establishing national standards for protecting sensitive patient health information.
- 2009: HITECH Act (Health Information Technology for Economic and Clinical Health Act) is passed, promoting the adoption of electronic health records and strengthening HIPAA enforcement.
- 2013: The Affordable Care Act (ACA) significantly impacts healthcare compliance, expanding coverage and introducing new regulations.
- Ongoing: The regulatory landscape continues to evolve with updates to HIPAA, new regulations addressing telehealth, AI, and big data, and increasing focus on data security and privacy.
Wrap-Up
Successfully achieving and maintaining compliance in healthcare isn’t a destination, but an ongoing process. It demands vigilance, a commitment to continuous improvement, and a proactive approach to risk management. By implementing robust systems, staying informed about regulatory changes, and fostering a culture of compliance within your organization, you can safeguard patient data, build trust, and ultimately, deliver the highest quality of care.
Remember, compliance isn’t just about avoiding penalties; it’s about upholding the ethical standards that define our profession.
FAQ Corner
What are the most common HIPAA violations?
Common HIPAA violations include unauthorized access or disclosure of protected health information (PHI), lack of proper security measures, and insufficient employee training.
How often should compliance audits be conducted?
The frequency of compliance audits depends on the size and complexity of the organization, but annual audits are generally recommended, with more frequent internal reviews.
What is the role of a compliance officer?
A compliance officer is responsible for developing and implementing the compliance program, conducting audits, training staff, and responding to compliance violations.
How can we improve employee compliance training?
Effective training involves interactive modules, regular refreshers, and clear communication of expectations and consequences.