What Are Conversation Overflow Cyberattacks and How Do They Work?
What are conversation overflow cyberattacks and how do they work? It’s a question that deserves a closer look, especially in today’s increasingly interconnected world. These attacks, unlike their more famous cousin the buffer overflow, exploit vulnerabilities in communication protocols, essentially flooding a system with excessive data until it crashes or reveals sensitive information. Think of it like a never-ending phone call that overwhelms the network, leaving it vulnerable to malicious manipulation.
We’ll delve into the mechanics, the vulnerabilities exploited, and most importantly, how to protect yourself and your systems.
This post will break down conversation overflow attacks in a digestible way, exploring how they differ from buffer overflows, the specific communication protocols often targeted, and the real-world consequences of a successful attack. We’ll cover the stages involved, from identifying vulnerabilities to crafting malicious input, and examine various prevention and mitigation strategies to keep your systems safe. We’ll even look at some case studies (without revealing sensitive information, of course!) to illustrate the real-world impact of these sophisticated attacks.
Defining Conversation Overflow Cyberattacks: What Are Conversation Overflow Cyberattacks And How Do They Work
Conversation overflow attacks, while less prevalent than their infamous cousin, the buffer overflow, represent a sneaky and potentially devastating type of cyberattack. They exploit vulnerabilities in how applications handle communication sessions, specifically the amount of data they’re designed to process within a single conversation. Think of it like a chat window that can only hold a certain number of messages; if you flood it with far more than it can handle, it might crash or behave unpredictably.Conversation overflow attacks differ from other attacks in their specific target: the communication session itself, rather than a specific memory buffer.
Unlike buffer overflows which directly manipulate memory locations, conversation overflows manipulate the parameters defining the conversation, such as the number of requests or the size of data packets. This manipulation can lead to denial-of-service conditions, information leaks, or even remote code execution, depending on the vulnerability exploited.
Conversation Overflow Attack Characteristics
Conversation overflow attacks hinge on exceeding the designed limits of a communication channel. This can involve sending an unusually large number of requests, exceeding the maximum allowed message size, or manipulating protocol headers to artificially inflate the size of the conversation. The core characteristic is the exploitation of a lack of robust input validation and error handling in the targeted application or system.
A well-designed system would reject or gracefully handle excessive input, preventing the overflow. The difference between a conversation overflow and a denial-of-service (DoS) attack lies in the
- mechanism*. DoS attacks often focus on flooding a system with requests, while conversation overflows target the
- handling* of those requests within a specific communication session, leveraging a specific vulnerability in the session management.
Comparison with Buffer Overflow Attacks
The following table contrasts conversation overflow and buffer overflow attacks:
| Attack Type | Mechanism | Target | Mitigation |
|---|---|---|---|
| Conversation Overflow | Exceeding limits of a communication session (e.g., number of requests, message size). | Communication session parameters and handling mechanisms. | Robust input validation, proper error handling, rate limiting, and secure session management. |
| Buffer Overflow | Writing data beyond the allocated memory buffer. | Memory buffers within an application. | Secure coding practices, compiler optimizations, address space layout randomization (ASLR), and data validation. |
Mechanisms of Conversation Overflow Attacks
Conversation overflow attacks, a sophisticated form of denial-of-service (DoS) attack, leverage vulnerabilities in communication protocols to overwhelm a target system with an excessive number of requests or messages. Understanding the mechanisms behind these attacks is crucial for developing effective defenses. These attacks don’t rely on exploiting a single, easily patched vulnerability; instead, they exploit the inherent limitations of how systems handle many simultaneous conversations.Attackers exploit vulnerabilities in communication protocols by sending malformed or excessively large packets, or by flooding the system with a massive number of legitimate-looking requests.
This overwhelms the system’s resources, leading to a denial of service for legitimate users. The effectiveness of these attacks hinges on the attacker’s ability to generate a high volume of traffic and to target protocols with weak or poorly implemented handling of concurrent connections.
Exploitation of Communication Protocol Vulnerabilities
Attackers carefully craft their malicious traffic to exploit weaknesses in how communication protocols manage resources and handle requests. For example, an attacker might send requests that require significant processing power or memory allocation from the server, thereby exhausting its resources. They might also exploit weaknesses in error handling, causing the system to crash or become unresponsive due to an inefficient error-handling mechanism.
The attacker’s goal is not necessarily to breach security directly but to disrupt normal operation by consuming all available resources. This renders the system unavailable to legitimate users, effectively creating a denial-of-service condition.
Susceptible Communication Protocols
Several communication protocols are susceptible to conversation overflow attacks. Protocols that lack robust mechanisms for rate limiting or connection management are particularly vulnerable. Examples include:
- HTTP/1.1: While HTTP/2 and later versions offer improvements, older implementations of HTTP/1.1 can be susceptible, especially if not properly configured with rate limiting or connection pooling.
- SMTP: Email servers using SMTP can be overwhelmed by a flood of connection requests or extremely large emails.
- SIP: Session Initiation Protocol, used in VoIP systems, can be targeted with attacks that flood the system with call setup requests.
- IMAP/POP3: Email retrieval protocols can be vulnerable to attacks that exhaust server resources by creating numerous connections or manipulating email size.
It’s important to note that even newer protocols can have vulnerabilities if not properly implemented or secured. The attack’s success relies less on specific protocol weaknesses and more on the sheer volume of requests and the target’s inability to handle them.
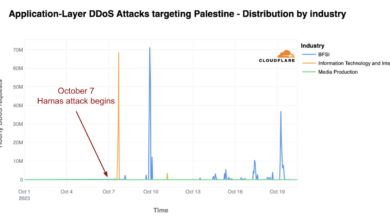
Real-World Examples of Conversation Overflow Attacks
While specific details of many conversation overflow attacks are not publicly disclosed for security reasons, the general principle has been observed in various denial-of-service attacks. For example, many large-scale DDoS attacks utilize a combination of techniques, and conversation overflow is often a component. Imagine a scenario where a website’s server is targeted with millions of simultaneous HTTP requests.
Even if each request is individually small, the sheer volume can overwhelm the server’s ability to process them, resulting in slow response times or complete unavailability. Similarly, an email server could be brought down by a massive influx of emails, each individually legitimate, but collectively exceeding the server’s capacity to handle them. These are simplified examples, but they illustrate the principle of conversation overflow attacks.
The key is the sheer volume of legitimate-seeming requests exceeding the server’s ability to handle them.
Exploiting Vulnerabilities

Conversation overflow attacks hinge on exploiting vulnerabilities in applications that handle user input, particularly those lacking robust input validation and buffer overflow protections. These vulnerabilities allow attackers to inject more data than the system is designed to handle, potentially overwriting critical memory regions and disrupting normal program execution. Understanding these vulnerabilities is key to preventing such attacks.Vulnerabilities that enable conversation overflow attacks are often found in applications written in languages like C or C++, which provide less inherent protection against buffer overflows compared to languages like Java or Python.
These vulnerabilities frequently stem from inadequate checks on the size of incoming data, allowing an attacker to inject excessively long strings or data structures. This can lead to a variety of problems, from application crashes to complete system compromise.
Types of Vulnerabilities
The most common vulnerability exploited in conversation overflow attacks is a lack of input validation. Applications should always verify the size and type of data received from users. Without this validation, attackers can easily inject malformed data that exceeds the allocated buffer size. Another vulnerability is the use of outdated or insecure libraries that don’t incorporate the latest buffer overflow protections.
Finally, insecure coding practices, such as failing to properly handle memory allocation and deallocation, can create exploitable vulnerabilities.
Crafting Malicious Input
Attackers craft malicious input by creating data strings or structures significantly larger than the application’s expected input size. This oversized data is designed to overflow the buffer, overwriting adjacent memory locations. The malicious data often includes shellcode—a small piece of code designed to execute arbitrary commands on the system. The attacker carefully constructs the payload to overwrite specific memory addresses, redirecting program execution to the injected shellcode.
Precise calculation of the buffer size and the placement of the shellcode are critical for a successful attack. This often involves reverse engineering the application to determine the exact memory layout.
Overflow and System Compromise
The overflow itself is not the attack; it’s the mechanism to gain control. Once the buffer overflows, the attacker’s injected code, usually the shellcode, overwrites critical program variables or return addresses on the stack. This allows the attacker to redirect the program’s execution flow to the malicious code. The shellcode then executes, granting the attacker various levels of access, from simple data exfiltration to complete system control.
This control can be used to steal sensitive information, install malware, or launch further attacks against other systems on the network.
Hypothetical Scenario: A Vulnerable Chat Application
Imagine a chat application written in C that doesn’t properly validate the length of user messages. An attacker could craft a message containing a significantly long string of characters, exceeding the buffer allocated for storing messages. This overflow overwrites the return address on the stack, redirecting execution to a malicious shellcode payload hidden within the oversized message. This shellcode could then grant the attacker access to the server’s file system, allowing them to download sensitive user data, including usernames, passwords, and chat logs.
The attacker might even gain root privileges, giving them complete control over the server. This scenario highlights the critical need for robust input validation and secure coding practices in applications that handle user-supplied data.
Impact and Consequences
A successful conversation overflow attack can have devastating consequences for individuals and organizations alike. The severity of the impact depends on several factors, including the target system’s criticality, the volume of injected data, and the attacker’s subsequent actions. The ramifications extend beyond simple data breaches; they can severely disrupt operations, damage reputation, and lead to significant financial losses.The potential consequences are far-reaching and can cascade through an organization, affecting various departments and stakeholders.
Understanding these potential impacts is crucial for implementing effective preventative measures and developing robust incident response plans.
Data Loss
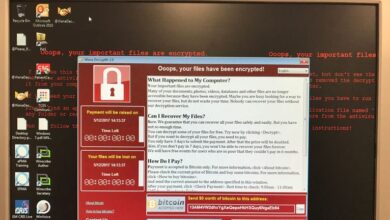
Conversation overflow attacks can lead to significant data loss. The sheer volume of malformed data injected into the system can overwhelm buffers and cause data corruption or overwriting of legitimate data. This could involve the loss of sensitive customer information, financial records, intellectual property, or internal communications. For example, a conversation overflow attack targeting a hospital’s patient management system could result in the loss of crucial medical records, potentially jeopardizing patient care and leading to legal ramifications.
The compromised data could include Personally Identifiable Information (PII), such as names, addresses, social security numbers, and medical histories, leading to identity theft and other serious consequences for affected individuals.
Service Disruption
Beyond data loss, conversation overflow attacks can cause significant service disruptions. The overflow of malformed data can crash applications, render systems unresponsive, and lead to extended downtime. This disruption can significantly impact an organization’s ability to conduct business, provide services, and meet its obligations. Imagine a large e-commerce platform suffering a conversation overflow attack; the resulting downtime could lead to lost sales, frustrated customers, and damage to the company’s reputation.
The extent of the service disruption depends on the criticality of the affected system and the duration of the outage. Recovery time can be lengthy and expensive, involving significant resources for system restoration and data recovery.
Financial Loss, What are conversation overflow cyberattacks and how do they work
The financial consequences of a conversation overflow attack can be substantial. These losses can stem from direct costs associated with incident response, data recovery, system repairs, and legal fees. There can also be indirect costs, such as lost revenue due to service disruptions, decreased customer trust, and potential regulatory fines. For instance, a financial institution suffering a successful attack resulting in the exposure of customer financial data could face significant fines under regulations like GDPR or CCPA, in addition to the costs of notifying affected customers and implementing remediation measures.
The reputational damage can also lead to a decline in customer loyalty and future business, resulting in long-term financial losses. The total cost can easily reach millions of dollars, depending on the severity of the attack and the organization’s size and industry.
Prevention and Mitigation Strategies
Preventing conversation overflow attacks requires a multi-layered approach focusing on secure coding practices, robust input validation, and secure communication protocols. Ignoring these crucial steps leaves systems vulnerable to exploitation and potentially devastating consequences. The following strategies are essential for mitigating this risk.
Effective prevention hinges on proactively strengthening the defenses of your systems, rather than simply reacting to attacks after they occur. This proactive approach minimizes the impact of vulnerabilities and ensures the overall security posture of your applications and infrastructure.
Secure Coding Practices
Secure coding is paramount in preventing conversation overflow attacks. Developers must meticulously avoid buffer overflows by employing techniques such as bounds checking, using safe string functions, and avoiding potentially dangerous functions like `strcpy` and `strcat`. Modern languages and libraries often provide safer alternatives that automatically handle memory allocation and bounds checking, minimizing the risk of buffer overflows. For example, languages like Java and C# manage memory automatically, reducing the likelihood of buffer overflow vulnerabilities.
In C++, using `std::string` instead of raw character arrays is a crucial step in enhancing security.
Securing Communication Protocols
Secure communication protocols play a vital role in preventing conversation overflow attacks. Employing protocols like TLS/SSL encrypts data transmitted between systems, preventing attackers from manipulating data in transit. Regular updates and patching of these protocols are crucial to address known vulnerabilities and ensure continued protection. Furthermore, implementing access control lists (ACLs) to restrict network access can limit the attack surface and prevent unauthorized access to vulnerable systems.
This controlled access prevents malicious actors from even attempting an attack.
Input Validation and Sanitization
Input validation and sanitization are critical for preventing a wide range of attacks, including conversation overflows. All user inputs, regardless of source, should be rigorously validated against expected formats and lengths. This validation should occur before any processing takes place. Sanitization involves removing or escaping potentially harmful characters, ensuring that even if an attacker manages to inject malicious data, it will be rendered harmless.
For instance, before storing user-supplied data in a database, it’s crucial to sanitize the input to prevent SQL injection attacks, a common vector for exploiting vulnerabilities that could indirectly lead to conversation overflows. This step acts as a crucial filter, preventing malicious code from executing.
Robust Error Handling
Robust error handling is a crucial component of secure software development. Proper error handling prevents attackers from gaining information about the system’s internal workings. Instead of displaying detailed error messages that reveal internal states, applications should provide generic error messages to users. Additionally, error logs should be carefully monitored for any suspicious activity that might indicate an attempted attack.
Thorough logging provides a detailed audit trail for post-incident analysis and helps in identifying potential vulnerabilities. This layered approach helps contain the damage from a successful attack and speeds up remediation efforts.
Case Studies and Examples
Analyzing real-world incidents helps illustrate the devastating consequences of conversation overflow attacks and the effectiveness of various mitigation strategies. While specific details of many attacks remain confidential due to security and legal reasons, we can examine generalized scenarios to understand the attack vectors and their impacts.Understanding the intricacies of conversation overflow attacks requires examining specific examples. While pinpointing precise details of real-world attacks is often restricted due to confidentiality agreements, we can explore a generalized case study to illustrate the mechanics and impact.
This hypothetical scenario draws upon common vulnerabilities and attack patterns observed in various systems.
A Hypothetical Conversation Overflow Attack
Imagine a system managing user interactions through a chat application. This application utilizes a buffer to store incoming messages. The buffer has a fixed size, let’s say 1024 bytes. A malicious actor crafts a message exceeding this limit, potentially including specially formatted characters designed to overwrite adjacent memory locations. Upon receiving this oversized message, the application fails to perform proper boundary checks, allowing the attacker’s data to overflow the buffer.
This overflow could overwrite crucial system variables, potentially leading to a crash or even allowing the attacker to execute arbitrary code. The attacker might exploit this to gain unauthorized access, steal data, or install malware. The impact would depend on the specific vulnerability exploited and the attacker’s goals. In this scenario, the attacker might gain complete control of the affected system.
Comparison of Conversation Overflow Attack Techniques
Different conversation overflow attacks employ various techniques, primarily varying in the payload’s composition and the targeted vulnerability. Some attacks might use simple long strings to overwhelm the buffer, while others use meticulously crafted payloads that include shellcode or other malicious instructions designed to execute specific commands upon buffer overflow. The success of an attack often depends on the sophistication of the payload and the vulnerability’s characteristics.
For instance, an attack targeting a web application might involve injecting JavaScript code into the overflown buffer to execute malicious scripts on the client-side, whereas an attack targeting a server-side application might involve injecting shellcode to gain control of the server.
Preventive Measures Against Conversation Overflow Attacks
Implementing robust preventive measures is crucial in mitigating the risks of conversation overflow attacks. Proactive steps are vital to ensure system security.
The following preventive measures have proven effective in mitigating similar attacks:
- Input Validation and Sanitization: Rigorously checking and sanitizing all user inputs before processing them is paramount. This involves limiting the length of inputs to prevent buffer overflows and removing or escaping potentially harmful characters.
- Secure Coding Practices: Employing secure coding practices, such as using bounds-checking functions and avoiding potentially unsafe functions, is essential. Developers should prioritize secure coding practices throughout the software development lifecycle.
- Regular Security Audits and Penetration Testing: Regularly conducting security audits and penetration testing can help identify and address potential vulnerabilities before they can be exploited by attackers.
- Using Safe Libraries and Frameworks: Utilizing well-vetted and secure libraries and frameworks can significantly reduce the risk of vulnerabilities. These libraries often incorporate built-in safeguards against common vulnerabilities, such as buffer overflows.
- Implementing Intrusion Detection and Prevention Systems (IDPS): IDPS can monitor network traffic and system activity for suspicious patterns indicative of a conversation overflow attack. Early detection enables timely intervention and mitigation.
Closing Notes
Understanding conversation overflow cyberattacks is crucial in today’s digital landscape. While they might not be as widely discussed as other attack vectors, their potential for damage is significant. By understanding the mechanisms behind these attacks, the vulnerabilities they exploit, and the preventative measures available, we can significantly strengthen our cybersecurity posture. Remember, proactive security is the best defense against these sophisticated threats.
Stay informed, stay vigilant, and stay safe!
Common Queries
What types of data are most vulnerable in a conversation overflow attack?
Sensitive data like login credentials, personally identifiable information (PII), financial records, and intellectual property are all at risk during a conversation overflow attack, as the system’s normal functioning is disrupted, potentially exposing stored data.
Can firewalls prevent conversation overflow attacks?
Firewalls can help, but they are not a complete solution. While they can filter malicious traffic, they may not be able to detect and prevent all conversation overflow attempts, especially sophisticated attacks that use legitimate communication protocols.
Are there any specific programming languages more susceptible to conversation overflow attacks?
No single language is inherently more susceptible, but vulnerabilities in how a language’s libraries or frameworks handle communication protocols can create exploitable weaknesses. Poorly written code that doesn’t properly validate or sanitize user input is the real culprit, regardless of the language used.