Healthcare Software Security Standards and Challenges
Healthcare software security standards and challenges are paramount in today’s digital age. Protecting sensitive patient data is critical, requiring robust security measures. From the design and development phases to incident response, navigating the complexities of HIPAA, NIST, and other frameworks is vital. This exploration delves into the standards, obstacles, and future of securing healthcare software.
This discussion covers the crucial aspects of healthcare software security, from the foundational principles and key standards to the practical challenges of implementation. We’ll explore the software development lifecycle (SDLC), data security, incident response, and emerging technologies impacting this critical field. Ultimately, this overview aims to equip readers with a comprehensive understanding of the multifaceted challenges and solutions involved in securing healthcare software.
Introduction to Healthcare Software Security: Healthcare Software Security Standards And Challenges
Protecting sensitive patient data and ensuring the smooth operation of healthcare systems are paramount in today’s digital age. Healthcare software, handling everything from diagnoses and treatments to billing and administrative tasks, has become indispensable. However, this reliance comes with a significant security risk, as vulnerabilities can lead to devastating consequences, including breaches of patient privacy, disruptions in care, and financial losses.
This necessitates a robust understanding of healthcare software security standards and the pervasive threats it faces.Healthcare software security is not merely a technical issue; it’s a matter of public trust and safety. The sensitive nature of patient information, combined with the critical role healthcare software plays in delivering care, demands an unwavering commitment to security. This commitment must encompass a comprehensive approach that addresses both technical safeguards and organizational policies.
Healthcare Software Security Standards
Healthcare software must adhere to stringent security standards to protect sensitive patient data. These standards are crucial for maintaining trust and compliance with regulations. Common standards like HIPAA (Health Insurance Portability and Accountability Act) and NIST (National Institute of Standards and Technology) frameworks provide a baseline for security practices. These frameworks, while differing in scope and focus, share a common goal: safeguarding patient data and ensuring the integrity of healthcare systems.
Critical Importance of Security in Healthcare
The importance of security in healthcare cannot be overstated. Patient data breaches can lead to severe consequences, ranging from identity theft and financial loss to reputational damage and a decline in public trust. Furthermore, disruptions in healthcare operations can lead to delays in treatment, potentially impacting patient health outcomes. A robust security posture is therefore a fundamental requirement for the responsible and ethical operation of any healthcare organization.
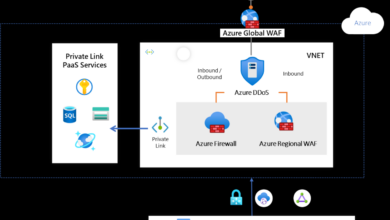
Healthcare software security standards are crucial, but implementing them effectively is a constant struggle. One area of concern is the reliance on cloud databases like Azure Cosmos DB, where vulnerabilities like those detailed in Azure Cosmos DB Vulnerability Details can significantly impact the security of sensitive patient data. Robust security protocols and regular audits are essential to mitigate these risks and ensure patient data remains protected.
Types of Threats and Vulnerabilities
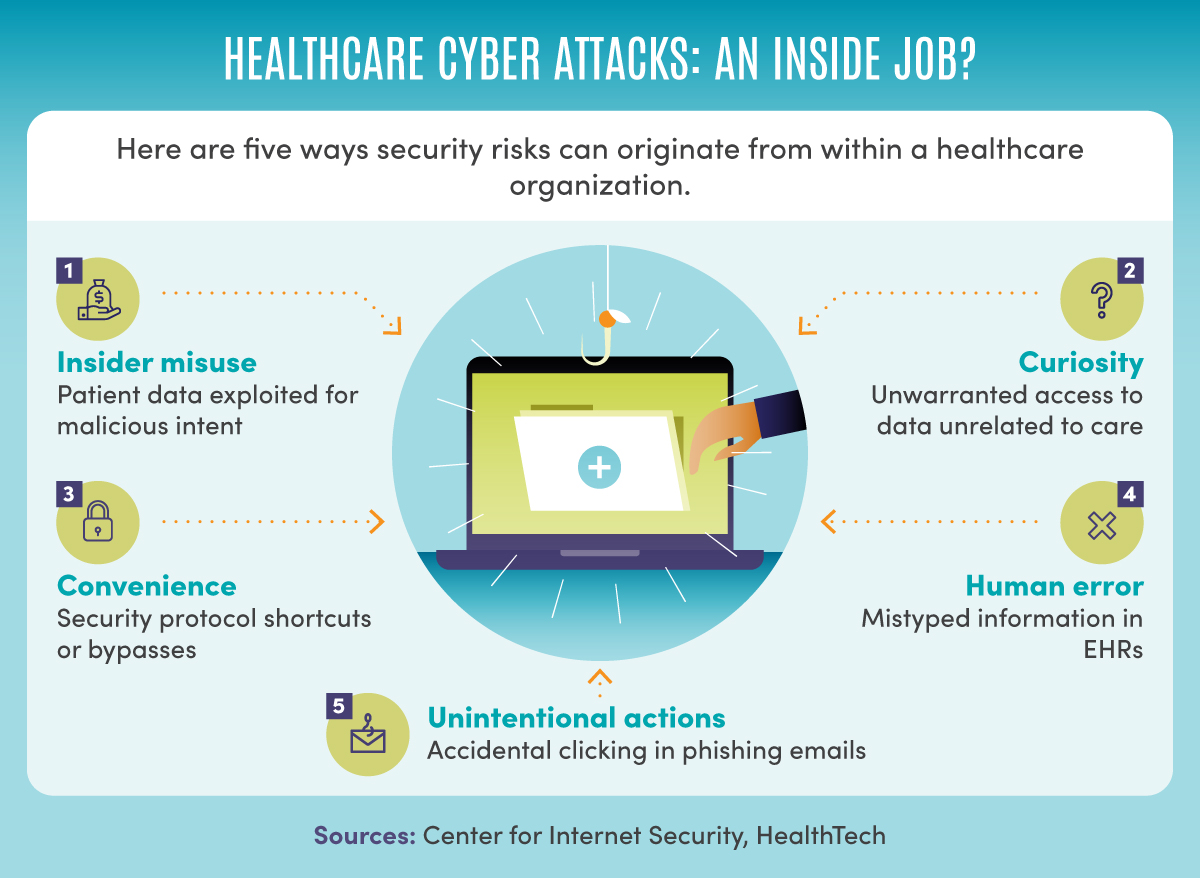
Healthcare software faces a multitude of threats and vulnerabilities. These range from malicious cyberattacks like ransomware and phishing attempts to vulnerabilities in software design and implementation. Insider threats, involving employees or contractors with malicious intent, also pose a significant risk. Moreover, vulnerabilities in third-party software integrated into healthcare systems can create entry points for attackers. These threats highlight the need for proactive security measures across the entire software lifecycle.
Real-World Security Breaches
Real-world examples of healthcare security breaches underscore the need for constant vigilance. These breaches often result in significant data losses, reputational damage, and financial repercussions for affected organizations. Understanding these breaches, while sobering, provides crucial insights into the evolving nature of cyber threats and the importance of proactive security measures. For example, a 2015 breach exposed millions of patient records, highlighting the potential for widespread damage when security protocols are inadequate.
Comparison of Healthcare Software Security Standards
| Standard | Focus | Key Requirements | Examples |
|---|---|---|---|
| HIPAA | Protecting patient health information | Security rule, privacy rule, breach notification rule | Encryption, access controls, audit trails |
| NIST Cybersecurity Framework | Overall cybersecurity posture | Identify, protect, detect, respond, recover | Risk assessment, vulnerability management, incident response plans |
This table provides a concise overview of key differences and commonalities between HIPAA and NIST. HIPAA focuses on the specific protection of patient data, while NIST offers a broader framework for managing cybersecurity across all aspects of an organization. Understanding these nuances is critical for developing a comprehensive security strategy.
Security Standards and Frameworks
Healthcare software, handling sensitive patient data, demands robust security measures. Establishing and adhering to recognized security standards is crucial for safeguarding patient privacy and ensuring the integrity of electronic health records (EHRs). These standards provide a framework for developers and organizations to build and operate secure systems, mitigating risks and promoting trust.Key principles underpinning healthcare software security standards revolve around confidentiality, integrity, and availability (CIA triad).
Healthcare software security standards are constantly evolving, presenting a complex challenge for providers. Recent developments, like the Department of Justice Offers Safe Harbor for MA Transactions here , highlight the need for robust security measures. This underscores the importance of staying ahead of evolving threats in the ever-changing landscape of healthcare software security.
These principles dictate how data is protected, maintained, and accessed, ensuring data is only viewable to authorized personnel. These principles also Artikel the necessary steps to maintain the accuracy and completeness of data, as well as ensuring access to systems when needed.
HIPAA Security Rule
The Health Insurance Portability and Accountability Act (HIPAA) Security Rule is a cornerstone of healthcare data security. It mandates specific safeguards for protecting electronic protected health information (ePHI). These safeguards cover administrative, physical, and technical safeguards, addressing various aspects of security. The rule’s requirements are designed to prevent unauthorized access, use, or disclosure of ePHI. Organizations must implement policies and procedures to ensure compliance.
This often includes access controls, audit trails, and regular security assessments.
NIST Cybersecurity Framework
The NIST Cybersecurity Framework provides a comprehensive structure for managing cybersecurity risks across various sectors, including healthcare. It offers a flexible approach, guiding organizations in identifying, assessing, and managing cybersecurity risks. This framework provides a common language and consistent approach for organizations to evaluate their security posture. It assists in the development of security policies, procedures, and controls that align with industry best practices and address emerging threats.
It emphasizes a risk-management approach, encouraging proactive measures to mitigate potential vulnerabilities.
Comparison of Security Frameworks
HIPAA focuses specifically on healthcare data protection, while the NIST Cybersecurity Framework offers a broader approach applicable to diverse sectors. HIPAA’s strength lies in its specific requirements for healthcare organizations, but it might lack the flexibility of the NIST framework for adapting to new technologies. The NIST framework, conversely, offers a more adaptable approach but might not address all the nuances of healthcare data protection as deeply as HIPAA.
Careful consideration of both frameworks is crucial for organizations seeking to implement comprehensive security measures.
Role of Compliance in Protecting Patient Data
Compliance with security standards, like HIPAA, is not merely a regulatory requirement but a critical component in protecting patient data. Adherence to these standards builds trust, fosters confidence in the healthcare system, and ultimately safeguards sensitive patient information. Compliance demonstrates a commitment to protecting patients’ rights and privacy. Non-compliance, on the other hand, carries significant penalties and reputational damage.
Influence on Software Design and Development
Security standards significantly influence the design and development of healthcare software. Security considerations must be integrated into every stage, from requirements gathering to deployment and maintenance. This often involves implementing robust access controls, encryption mechanisms, and secure coding practices. Secure development lifecycle (SDL) methodologies are often used to ensure security is prioritized throughout the software development process.
Key Requirements of HIPAA for Healthcare Software
| Category | Key Requirements |
|---|---|
| Administrative Safeguards | Security policies, risk assessments, workforce training, incident response plan |
| Physical Safeguards | Protecting physical access to systems, facilities, and data |
| Technical Safeguards | Access controls, encryption, audit trails, business continuity plans, system activity logs |
Challenges in Implementing Security Standards
Implementing robust security standards in healthcare software is crucial, but fraught with obstacles. The sensitive nature of patient data necessitates stringent protections, yet healthcare organizations face significant hurdles in achieving and maintaining these safeguards. These challenges are not only technical but also organizational, stemming from the dynamic nature of technology and the inherent complexities of healthcare operations.
Common Obstacles in Implementation
The path to secure healthcare software is often paved with difficulties. Budget constraints, limited technical expertise, and the sheer complexity of integrating security measures into existing systems are frequently encountered obstacles. A lack of clear security policies and procedures, coupled with a shortage of trained personnel to enforce them, further complicates the process. Additionally, a lack of readily available resources for security training and awareness programs within organizations can hinder the adoption of best practices.
Maintaining Security in Evolving Technological Landscapes
Rapid technological advancements present a constant challenge to maintaining security. New vulnerabilities are discovered and exploited regularly, requiring constant adaptation and updates to existing systems. Healthcare organizations must keep pace with evolving threats and ensure that their security measures are effective against the latest attacks. This ongoing adaptation is crucial to prevent outdated systems from becoming points of weakness.
The introduction of new technologies, like cloud computing and mobile devices, necessitates adjustments to security protocols to safeguard sensitive data.
Ensuring Data Integrity and Confidentiality in EHRs
Electronic Health Records (EHRs) are critical for modern healthcare, but safeguarding the integrity and confidentiality of the data they contain is a significant concern. Data breaches, unauthorized access, and the risk of data corruption can have serious consequences for patient care and organizational reputation. EHR systems must incorporate robust encryption methods, access controls, and regular security audits to minimize these risks.
Maintaining data integrity is also vital to ensure accuracy in patient records, impacting diagnosis and treatment.
Managing and Responding to Security Incidents
A comprehensive security strategy must address the potential for security incidents. Organizations must have well-defined procedures for detecting, responding to, and recovering from security breaches. The speed and efficiency of incident response directly impact the damage inflicted by a breach. Effective incident management involves clear communication channels, rapid escalation procedures, and a plan for restoring systems and data to a functional state.
Common Security Misconfigurations and Vulnerabilities
Security misconfigurations and vulnerabilities in healthcare software often stem from overlooked details. Improperly configured firewalls, outdated software, and weak passwords are common examples. Lack of regular security patching and inadequate access controls are other key vulnerabilities. Failure to adhere to security best practices, such as least privilege access, can create significant security risks.
Top 5 Security Challenges Faced by Healthcare Organizations
| Rank | Challenge | Description |
|---|---|---|
| 1 | Budgetary Constraints | Limited resources for implementing and maintaining security measures. |
| 2 | Lack of Skilled Personnel | Shortage of security experts to design, implement, and maintain security systems. |
| 3 | Evolving Technology Landscape | Adapting to new technologies and threats in a rapidly changing environment. |
| 4 | Data Integrity and Confidentiality | Ensuring the accuracy and security of patient data within EHR systems. |
| 5 | Security Incident Management | Developing and executing effective procedures for detecting, responding to, and recovering from breaches. |
Software Development Lifecycle (SDLC) and Security
Building secure healthcare software requires a proactive approach integrated throughout the entire software development lifecycle (SDLC). Ignoring security at any stage can lead to vulnerabilities that compromise patient data and trust. This necessitates a shift-left strategy, bringing security considerations into every phase of development, from initial planning to final deployment.
Role of Security in the SDLC
Security is not an afterthought but an integral component of every phase in the SDLC. It involves establishing security requirements, developing secure code, conducting rigorous testing, and implementing robust security measures throughout the system’s lifespan. Early involvement minimizes the risk of costly rework and potential breaches later on.
Best Practices for Integrating Security into the SDLC
Effective integration of security requires a shift-left approach, emphasizing security awareness and best practices from the outset. This includes:
- Security Requirements Definition: Defining clear security requirements from the initial project planning phase ensures that security considerations are embedded into the design and architecture. This ensures alignment between security goals and functional requirements.
- Secure Coding Practices: Implementing secure coding guidelines and training developers on secure coding practices reduces the occurrence of common vulnerabilities in the source code. This minimizes the potential for exploits and unauthorized access.
- Security Testing Throughout the SDLC: Integrating security testing (penetration testing, vulnerability scanning) at every stage of the SDLC uncovers vulnerabilities early on, allowing for timely fixes and preventing costly problems later.
Security Testing and Audits
Security testing and audits are crucial for identifying vulnerabilities in the software. These should be incorporated throughout the SDLC:
- Static Analysis: Examining the codebase for vulnerabilities without executing the code helps find issues in design and implementation. Tools like SonarQube and Checkmarx perform static analysis, identifying potential flaws.
- Dynamic Analysis: Executing the code under controlled conditions, simulating real-world attacks and user interactions, helps uncover vulnerabilities that static analysis may miss. Tools like Burp Suite and OWASP ZAP automate dynamic analysis.
- Penetration Testing: Emulating real-world attacks to identify potential weaknesses in the system. Professional penetration testers use specialized tools and techniques to test the system’s resilience.
Security Tools and Techniques
Integrating security tools and techniques into the SDLC is essential for efficient vulnerability identification and remediation.
- Security Information and Event Management (SIEM) Systems: These systems monitor and analyze security events, helping detect and respond to security incidents. Examples include Splunk and ELK Stack.
- Vulnerability Scanning Tools: Tools like Nessus and OpenVAS automatically scan systems and applications for known vulnerabilities, allowing for proactive mitigation.
- Security Information and Event Management (SIEM) Systems: These systems monitor and analyze security events, helping detect and respond to security incidents. Examples include Splunk and ELK Stack.
Secure Coding Practices in Healthcare Software
Healthcare software demands specific secure coding practices due to the sensitive nature of patient data. These include:
- Data Validation: Rigorous input validation prevents malicious data from corrupting the system or exposing sensitive information.
- Authentication and Authorization: Implementing strong authentication and authorization mechanisms restricts access to sensitive data based on user roles and permissions.
- Data Encryption: Encrypting sensitive data both in transit and at rest protects it from unauthorized access.
SDLC Stages and Security Considerations
| SDLC Stage | Security Considerations |
|---|---|
| Requirements Gathering | Define security requirements, identify potential risks, and establish security controls. |
| Design | Design secure architectures, implement secure protocols, and identify potential vulnerabilities. |
| Implementation | Write secure code, adhere to coding standards, and incorporate security features. |
| Testing | Perform various security tests (penetration testing, vulnerability scanning), identify and address vulnerabilities. |
| Deployment | Deploy secure infrastructure, configure security settings, and implement access controls. |
| Maintenance | Monitor security, update security patches, and respond to security incidents. |
Data Security and Privacy in Healthcare Software

Protecting patient data is paramount in healthcare software. The sensitive nature of this information necessitates robust security measures to ensure confidentiality, integrity, and availability. This involves not only encryption and access control but also meticulous attention to the entire software development lifecycle. Failure to implement these measures can lead to significant financial and reputational damage, as well as potential legal repercussions.
Importance of Data Encryption and Access Control
Data encryption and access control are fundamental components of a secure healthcare software system. Encryption transforms data into an unreadable format, preventing unauthorized access. Access control mechanisms regulate who can view, modify, or delete data, limiting potential breaches. Strong encryption and access controls create a secure environment for sensitive patient information, ensuring only authorized personnel can access it.
Ensuring Data Confidentiality, Integrity, and Availability
Confidentiality ensures that only authorized individuals can access patient data. Integrity guarantees that data is accurate and complete. Availability ensures that authorized users can access data when needed. These three pillars are crucial for safeguarding patient information and maintaining the reliability of healthcare software. To achieve this, multiple layers of security are required, ranging from encryption protocols to robust authentication systems.
Secure Authentication Mechanisms
Secure authentication mechanisms verify the identity of users attempting to access healthcare software. These mechanisms include strong passwords, multi-factor authentication (MFA), and biometric identification. Multi-factor authentication adds an extra layer of security by requiring multiple forms of verification (e.g., password plus a code sent to a mobile phone). This significantly reduces the risk of unauthorized access.
Data Encryption Methods
Various encryption methods exist, each with its strengths and weaknesses. Examples include Advanced Encryption Standard (AES), which is a widely used symmetric encryption algorithm. RSA is an asymmetric encryption method frequently employed for digital signatures and key exchange. The choice of encryption method depends on the specific security requirements and the sensitivity of the data being protected.
Protecting Sensitive Patient Data from Unauthorized Access
Protecting sensitive patient data requires a multi-faceted approach. This includes implementing robust access control lists, regular security audits, and employee training on security protocols. Strong passwords, combined with multi-factor authentication, help prevent unauthorized access. Regular security audits help identify vulnerabilities and address potential threats.
Data Security Measures and Effectiveness
| Data Security Measure | Effectiveness | Description |
|---|---|---|
| Strong Passwords | High | Complicated passwords with a combination of uppercase and lowercase letters, numbers, and symbols. |
| Multi-Factor Authentication (MFA) | Very High | Requires multiple forms of verification, such as a password and a code sent to a mobile phone. |
| Regular Security Audits | High | Identify vulnerabilities and potential threats in the system. |
| Data Encryption | High | Transform data into an unreadable format using encryption algorithms. |
| Access Control Lists (ACLs) | High | Define who can access specific data or functionalities. |
| Employee Training | Moderate to High | Educate employees on security protocols and best practices. |
Effective data security requires a layered approach that combines multiple security measures.
Security Incident Response and Management
Healthcare software, handling sensitive patient data, demands robust security incident response plans. A well-defined plan minimizes damage, maintains patient trust, and safeguards the organization’s reputation. A proactive approach is crucial to quickly identify, contain, and recover from security breaches, ultimately ensuring the confidentiality, integrity, and availability of sensitive data.
Importance of Incident Response Planning
A comprehensive incident response plan is essential for healthcare software. It acts as a roadmap, outlining procedures for handling security incidents. This pre-defined strategy minimizes response time, ensures consistent actions, and facilitates effective communication during critical situations. A well-structured plan allows healthcare organizations to maintain operational continuity, safeguard patient data, and prevent escalation of damage.
Steps to Take in Case of a Security Breach
Immediate action is paramount when a security breach occurs. The first step involves containing the incident to prevent further spread. This includes isolating affected systems, temporarily halting access, and preserving evidence for investigation. A coordinated response involving IT security teams, legal counsel, and potentially external experts is vital. Maintaining communication with affected parties is critical to addressing their concerns.
Step-by-Step Procedure for Handling a Security Incident
A structured approach streamlines incident handling. The initial step involves identifying and confirming the incident. Next, contain the impact by isolating affected systems and data. Preserve evidence meticulously. Assess the impact and scope of the breach, then analyze the cause and identify vulnerabilities.
Develop and implement a recovery plan to restore systems and data. Finally, conduct a post-incident review to identify areas for improvement in the security posture.
Role of Security Monitoring Tools and Technologies
Security monitoring tools play a crucial role in detecting and responding to security incidents. These tools track system logs, network traffic, and user activities for anomalies. Intrusion detection systems (IDS) and intrusion prevention systems (IPS) are essential for identifying malicious activities in real-time. Security information and event management (SIEM) systems consolidate security logs and provide a central platform for incident analysis.
Process of Reporting and Investigating Security Incidents
A clear reporting and investigation process is crucial for efficient incident handling. Immediately report security incidents to relevant stakeholders, including management and regulatory bodies. A formal investigation process, following established protocols, should be initiated. The investigation should meticulously collect evidence, identify the cause, and determine the extent of the damage. Lessons learned from the incident should be documented for future prevention.
Key Steps in a Security Incident Response Plan
| Step | Description |
|---|---|
| 1. Preparation | Developing a comprehensive incident response plan, training personnel, and establishing communication channels. |
| 2. Identification | Detecting and confirming a security incident. |
| 3. Containment | Isolating the affected systems and data to prevent further damage. |
| 4. Eradication | Removing the threat and restoring systems to a secure state. |
| 5. Recovery | Restoring systems and data to their previous operational state. |
| 6. Post-Incident Activity | Evaluating the incident, identifying lessons learned, and improving the incident response plan. |
Future Trends and Emerging Technologies
The healthcare software landscape is rapidly evolving, driven by technological advancements that promise to revolutionize patient care and enhance security. This transformation necessitates a proactive approach to security, anticipating and mitigating the risks associated with new technologies. Understanding the future of healthcare software security is crucial for ensuring the continued safety and integrity of sensitive patient data.
The Impact of Artificial Intelligence and Machine Learning
AI and machine learning (ML) are increasingly integrated into healthcare software, automating tasks, improving diagnostics, and personalizing treatment plans. This integration, while beneficial, introduces new security challenges. AI systems can be vulnerable to adversarial attacks, where malicious inputs can manipulate the system’s decision-making processes. For example, a fraudulent actor might craft a medical image that tricks an AI-powered diagnostic tool into misinterpreting a benign condition as a severe illness.
Robust training data and rigorous testing are critical to mitigate such vulnerabilities. Furthermore, the need to protect the training data itself, often comprising sensitive patient information, becomes paramount.
Cloud Computing in Healthcare
Cloud computing is transforming healthcare software delivery, offering scalability, cost-effectiveness, and accessibility. However, the security implications of storing sensitive patient data in cloud environments require careful consideration. Healthcare organizations must select cloud providers with strong security measures, adhering to industry standards and regulations like HIPAA. Compliance with data encryption and access controls is vital. Data breaches in the cloud can have devastating consequences, leading to reputational damage, financial penalties, and compromised patient trust.
Implementing multi-factor authentication, secure access management, and regular security audits are crucial for mitigating risks.
Blockchain Technology for Enhanced Security, Healthcare software security standards and challenges
Blockchain technology offers a decentralized and immutable record-keeping system, potentially enhancing data security and integrity in healthcare software. It can be employed to securely store and manage patient records, ensuring data authenticity and preventing tampering. For example, a blockchain-based system could track the provenance of medical devices, guaranteeing their authenticity and safety. The technology holds great promise for secure data sharing among healthcare providers, enabling efficient and reliable communication while protecting patient privacy.
However, the complexity of implementing blockchain solutions requires careful planning and expertise.
Healthcare software security standards face a lot of hurdles, from protecting patient data to ensuring reliable operations. A big part of the challenge is ensuring the code itself is secure. This directly relates to the need for robust safety measures, like those discussed in the article “Deploying AI Code Safety Goggles Needed” Deploying AI Code Safety Goggles Needed.
Ultimately, addressing these issues in software development is critical to achieving the highest level of security for healthcare systems.
Security Implications of the Internet of Medical Things (IoMT)
The proliferation of interconnected medical devices, collectively known as the Internet of Medical Things (IoMT), introduces new avenues for cyberattacks. These devices, often with limited processing power and security features, can become vulnerable entry points for malicious actors. A compromised IoMT device could potentially disrupt patient care or expose sensitive patient data. Security protocols for IoMT devices must prioritize robust authentication, encryption, and regular updates to patch vulnerabilities.
Careful consideration of device security throughout the entire lifecycle, from design to disposal, is crucial.
Future Trends in Healthcare Software Security
| Trend | Description | Impact ||—|—|—|| AI-driven security | AI algorithms can detect and respond to threats in real time, enhancing the effectiveness of security systems. | Improved threat detection and response. || Zero trust security models | This approach assumes no implicit trust, verifying every user and device before granting access. | Reduced attack surface. || Enhanced data encryption and anonymization | Advanced encryption methods and anonymization techniques protect sensitive data during transmission and storage.
| Increased data protection. || Cybersecurity awareness training | Educating healthcare professionals and staff about cybersecurity threats and best practices. | Improved user awareness and behavior. || DevSecOps integration | Embedding security practices into the software development lifecycle. | Improved security at all stages of software development.
|
Final Summary
In conclusion, securing healthcare software requires a multi-faceted approach encompassing robust standards, proactive implementation strategies, and adaptability to emerging technologies. Addressing the challenges head-on, through careful consideration of the entire software development lifecycle, data security, and incident response, is essential for protecting patient data and maintaining trust in the digital healthcare landscape. The future of healthcare software security hinges on embracing innovation while upholding the highest standards of patient data protection.
Key Questions Answered
What are some common security misconfigurations in healthcare software?
Common misconfigurations include weak passwords, inadequate access controls, insecure APIs, and outdated software. Failing to patch vulnerabilities promptly also presents a significant risk.
How does the cloud impact healthcare software security?
Cloud computing presents both opportunities and challenges. While it can offer scalability and cost-effectiveness, it’s crucial to implement robust security measures within the cloud environment to protect sensitive patient data from breaches. Selecting a reliable cloud provider and configuring security settings appropriately are paramount.
What role does AI play in healthcare software security?
AI can enhance security by automating threat detection and response. Machine learning algorithms can identify anomalies and patterns indicative of potential breaches, enabling faster response times. However, ethical considerations and the potential for bias in AI models need careful attention.
What are the key requirements of HIPAA for healthcare software?
HIPAA mandates the protection of Protected Health Information (PHI). Key requirements include implementing safeguards for access control, encryption, audit trails, and regular security assessments. Organizations must ensure their software complies with these regulations.